Frozen Shoulder, Management and Cause
- by Joanna Blair
- •
- 15 Jan, 2023
- •
Pathology, Cause & Treatment

The typical patient that develops adhesive capsulitis are women aged between 50 to 70 and has been reported to occur within both shoulders simultaneously in up to 40-50% of patients. Adhesive capsulitis is commonly associated with other systemic and nonsystemic conditions. By far the most common is the co-morbid condition of diabetes mellitus, with an incidence of 10–36%.
Codman (1934) was the first to describe AC and the common criteria shared by individuals with frozen shoulder which include the slow onset of pain, inability to sleep on the affected side, painful and restricted shoulder abduction and external rotation motions. Plain x-rays of shoulders with AC may range from a normal appearance to osteopenic or degenerative changes (2).
Other co-morbid conditions include hyperthyroidism, hypothyroidism, hypoadrenalism, Parkinson’s disease, cardiac disease, pulmonary disease, stroke, and even surgical procedures that do not affect the shoulder such as cardiac surgery, cardiac catheterization, neurosurgery, and radical neck dissection.
Duration
Clinical Phases (6):
The condition progresses in three stages:
1. Freezing; pain is most severe during this phase. This inflammatory phase typically lasts between 3 and 9 months. The stage is characterised by an acute synovitis of the glenohumeral joint, when the synovium or of the connective tissue that lines the inside of the joint capsule becomes inflamed.
2. Frozen or adhesive, stiff phase whereby the pain gradually reduces but the range of motion in all planes becomes severely restricted. This stage lasts anywhere 4 to 12 months.
3. Thawing or recovery phase involves the gradual spontaneous improvement of shoulder function (5-26 months).
Cause; Primary & Secondary Frozen Shoulder
Primary adhesive capsulitis is idiopathic with the cause being unknown and classified to patients who present with no significant findings within their case history, clinical examination, or radiographic evaluation to explain their loss of joint motion and pain (1).
Primary idiopathic frozen shoulder can be associated with other diseases and conditions such as diabetes mellitus and might be the first presentation of a diabetic patient. Patients with systemic diseases such as thyroid, cardiovascular and lung diseases along with open heart surgery, depression, polymyalgia and Parkinson’s disease are also at higher risk.
Patients with secondary adhesive capsulitis disclose a trauma or surgery to the affected upper extremity prior to their shoulder symptomatology (1).
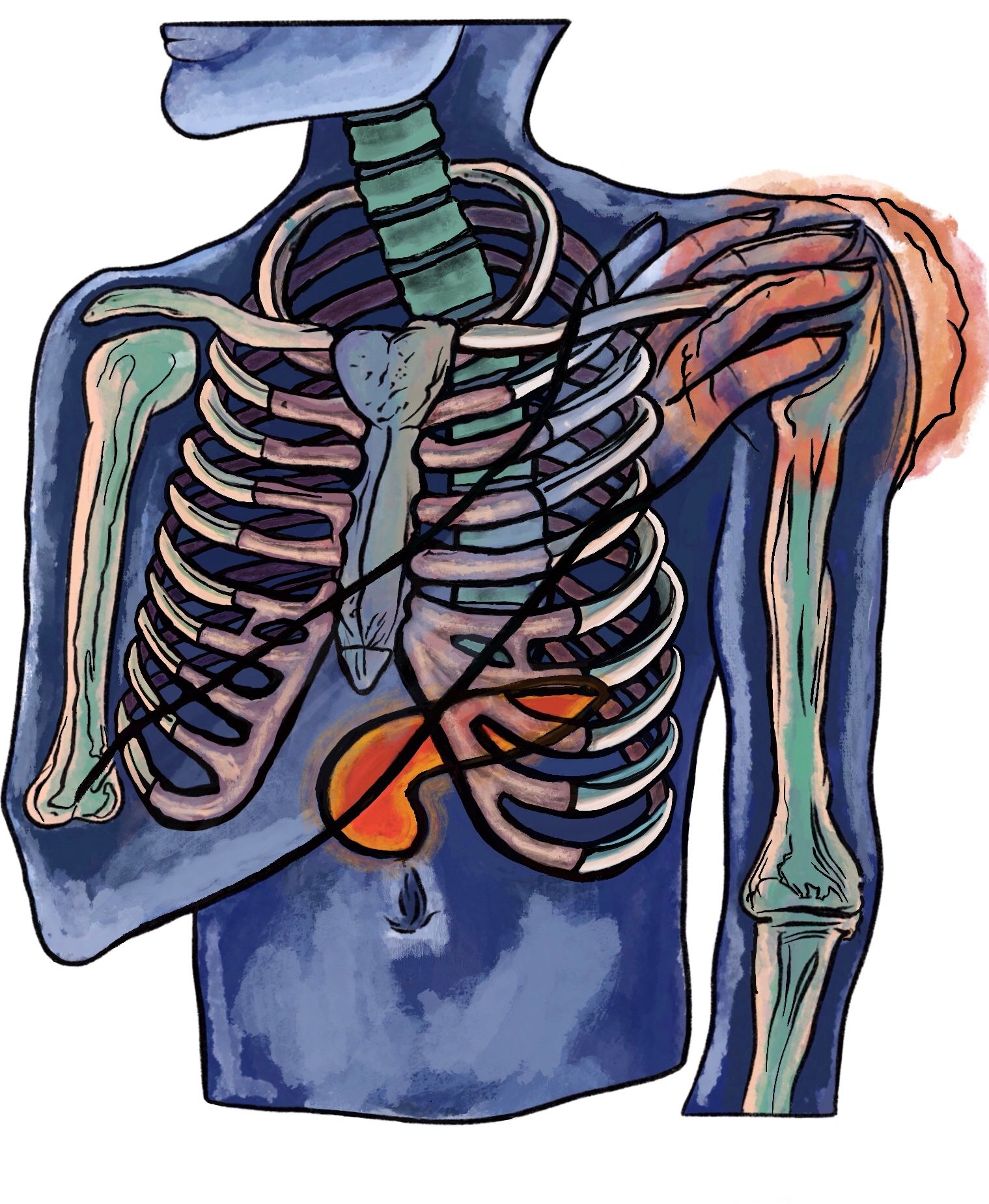
The Pancreas, Diabetes & Shoulder Problems
The pancreas is a large gland located behind the stomach and has the function of maintaining healthy blood sugar levels by producing insulin, glucagon and other hormones (5).
Diabetes is a metabolic condition characterised by hyperglycemia caused by insulin deficiency and / or impaired effectiveness of insulin action. The disease is considered one of the most challenging and disabling health problems in the 21st century with being the fifth leading cause of death in most developed countries (1).
The disease can be classified into two main types. Type 1 diabetes (T1D) is an organ-specific autoimmune disease caused by an autoimmune response against pancreatic islet beta cells which results to the loss of insulin production (1). Type 2 diabetes occurs from insulin deficiency and/ or insulin resistance (1). Diabetic patients are five time more likely than nondiabetic patients to develop frozen shoulder (1).
Classic Warning Signs and Symptoms for Diabetes
Polyuria (increased urination), polydypsia (increased thirst) and polyphagia (increased hunger) which occurs commonly in type 1 and 2 diabetes with very high levels of hyperglycaemia are usually clear signs and symptoms. Severe weight loss is common only in type 1 diabetes or if type 2 diabetes remains undetected for a long period. Unexplained weight loss, fatigue, irritability and restlessness and body pain are also common signs of undetected diabetes. The condition can be difficult to catch as symptoms can be mild or have a gradual development and remain unnoticed.
Other signs and symptoms include (3):
- Repeated infections especially in the genital areas, urinary tract, skin, oral cavity and delayed wound healing.
- Dry mouth
- Burning, pain, numbness on the feet along with Itching.
- Reactive hypoglycaemia
- Acanthoses nigricans or the presence of velvety dark patches of the neck, arm pit, groin which is an indication of insulin resistance.
- Reduced vision
- Impotence or erectile dysfunction
Advanced Glycation End Products or AGES are proteins or lipids that become glycated by having an added sugar molecule after having undergone glycation. Glycation end products are believed to play a causative role in the vascular complications of diabetes mellitus. In diabetic tissue, hyperglycemia can cause a non-enzymatic covalent bonding of sugar molecules to collagen fibers. Over time, AGEs increase the cross linking of collagen fibres of the shoulder capsule, thus changing the mechanical properties of tissue by making the structures stiffer and weaker (1).
Management
As Ben-Arie et al., (2020) highlight, there is still disagreement upon which treatment is the most effective for reducing pain and restoring ROM for patients with FS but most research has found strong evidence in favor of laser therapy and steroid injections for pain treatment in the short term (4).
How Might Physical Therapy Modalities Help?
Massage modalities can be applied with the aim to increase blood circulation, relieve pain by interfering with pain signals' pathway to the brain via the 'gate control theory', stimulate the release of endorphins, encourage lymphatic drainage, relieve muscle tension and spasms.
Dry Cupping
Two case studies investigated the effectiveness of dry cupping (hijamah) whilst individuals were in phase two of having adhesive capsulitis. Suctioning of cups with gliding techniques were applied at the affected areas (1, 8).
The treatment modality aims to encourage blood flow to the area and increase the permeability of blood vessels which helps aid exudation of plasma proteins and fluid into the tissue to create swelling or oedema (1). The vacuum technique also aims to help the circulation of lymphatic fluid, reduce inflammation and facilitate recruitment of immune cells and support the healing process (1). Both case studies found significant improvements with reduced pain levels, active range of joint movement and muscular tenderness.
Acupuncture
A systematic review and a meta-analysis by Ben-Arie et al., (2020) concluded that acupuncture had shown to be a safe treatment with a significant effect in regard to reducing pain, improving shoulder function, and flexion ROM in the short term and midterm after analysing a total of 966 FS patients from 13 publications (4).
References
- Abicd, M., Shazia, H., Khan, S., Nazli, T., Mahto, R. R. (2021) Effect of Hijamah (Dry Cupping) on Frozen Shoulder: A Case Study, Journal of Advanced Research in Ayurveda, Yoga, Unani, Sidhha & Homeopathy, 8; (1,2): 14-17.
- Alsubheen, S. A., MacDermid, J. C., Overend, T. J. Faber, K. J. (2019) The Diabetic Shoulder – A Literature Review, J Diabetes Clin Res., 1; 2: 59-70.
- Ambady, R. (2014) Know the Signs and Symptoms of Diabetes, Indian Journal Medical Research, 579-581.
- Ben-Arie, E., Kao, P-Y ., Lee, Y-C., Ho, W-C., Chou, L-W., Liu, H-P. (2020) The Effectiveness of Acupuncture in the Treatment of Frozen Shoulder: A Systematic Review and Meta-Analysis, Hindawi, Evidence-Based Complementary and Alternative Medicine: 1-14.
- Chan, H. B. Y., Pua, P. Y., How, C. H. (2017) Physical Therapy in the Management of Frozen Shoulder, SMJ, 58 (12): 685–689.
- Hsu, C. L., H‐H Sheu, W. (2016) Diabetes and Shoulder Disorders, 7(5): 649–651.
- Hwanga, K. R., Murrell, G. A. C., Millar, N, L., Bonar, F., Lam, P., Walton, J. R. (2015) Advanced glycation end products in idiopathic frozen shoulders, J Shoulder Elbow Surg., 25; 6: 981–988.
- Imam, H., Ishtiyaque. Alam, M. I., Perveen, A., Goswami, A., Khan, Q., Ahmad, T. (2019) Management of Frozen Shoulder with Oil Cupping Massage: A Case Study, Journal of Applied Sciences, 2; (2): 49-53.
- Kawasaki, E., (2014) Type 1 Diabetes and Autoimmunity, Clin Podiatry Endocrinol, 23; (4): 99-105.
- Manske, R. C., Prohaska, D. (2008) Diagnosis and Management of Adhesive Capsulitis. Curr Rev Musculoskelet Med 1(3–4): 180–189.
- Serna, de la D., Navarro-Ledesma, S. N., Alayón, F., López, E., Pruimboom. L. (2021)
- A Comprehensive View of Frozen Shoulder: A Mystery Syndrome., Frontiers In Medicine, 8; 663703: 1-10.
- Whelton, C., Peach, C. A. (2017) Review of Diabetic Frozen Shoulder, Eur J Orthop Surg Traumatol, Springer.