The Trigeminal Nerve, Facial Pain & Trigeminal Neuralgia
- by Joanna Blair
- •
- 15 Feb, 2022
- •
The Trigeminal Nerve & Trigeminal Neuropathy
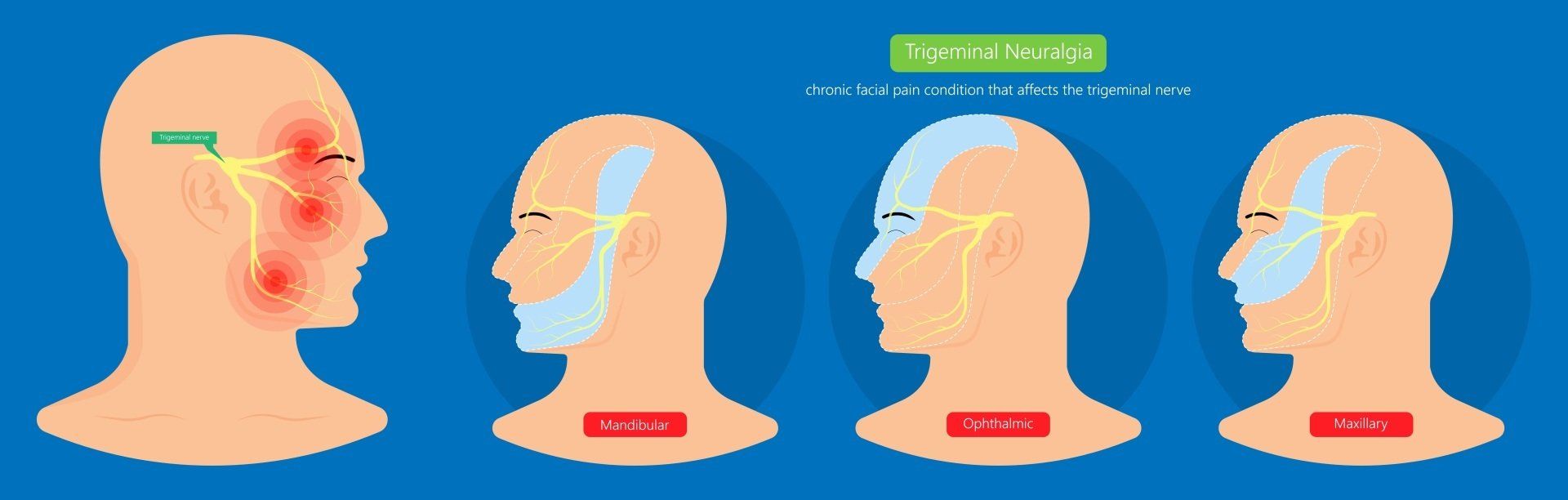
Trigeminal neuralgia (TN) is a common type of severe chronic facial disorder characterised by brief electric shock-like (paroxysmal) pains in one or more divisions of the fifth cranial nerve. The condition is also termed 'tic douloureux' as the pain can cause individuals to distort or wince their face from the severe pain (7). The intense pain in the face caused by TN is also known as the 'Suicide Disease' or Fothergill's disease.
The maxillary and mandibular nerves are the lower two branches of the Trigeminal nerve and most commonly affected. TN reportedly has an annual incidence of 4 and 27 per 100,000, the pain is commonly unilateral and may be mistaken for dental problems (9).
The International Association for the Study of Pain (IASP) defined TN as “a sudden, usually unilateral, severe, brief stabbing and recurrent episode of pain in the distribution of one or more branches of the fifth cranial nerve” (9). The frequency, duration, and severity of these painful attacks gradually increase and often become resistant to medication. The neuralgia can often become chronic and severely affect the quality of life, cause cognitive disturbances such as anxiety and depression in patients with TN (9).
Symptomatology
Symptoms of TN are excruciating pain that can be triggered by light touch or mild stimulation from normal activities such as (11):
- Brushing teeth
- Talking
- Chewing
- Applying make up
- Encountering a light breeze
- Smiling
- Touching the skin lightly
- Washing
- Shaving
- Blowing the nose
- Drinking hot or cold beverages
In the early stages of this condition the individual may experience short, mild attacks. But trigeminal neuralgia can progress and cause longer, more-frequent periods of searing pain. Overall, women are more affected by this condition than men with an average age above fifty (13).
Anatomy of the Trigeminal Nerve
- The mylohyoid
- Anterior belly of digastric
- Tensor tympani
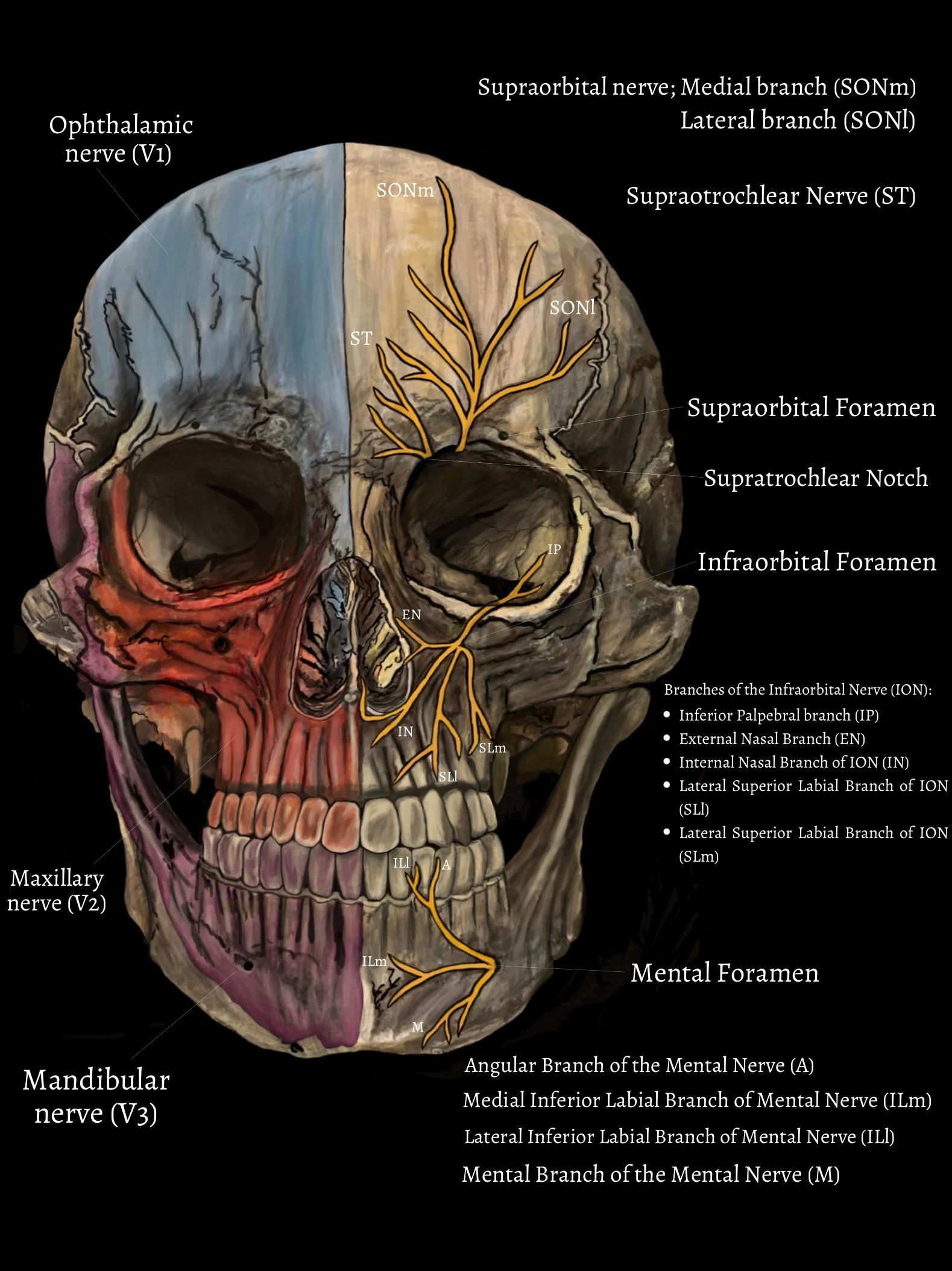
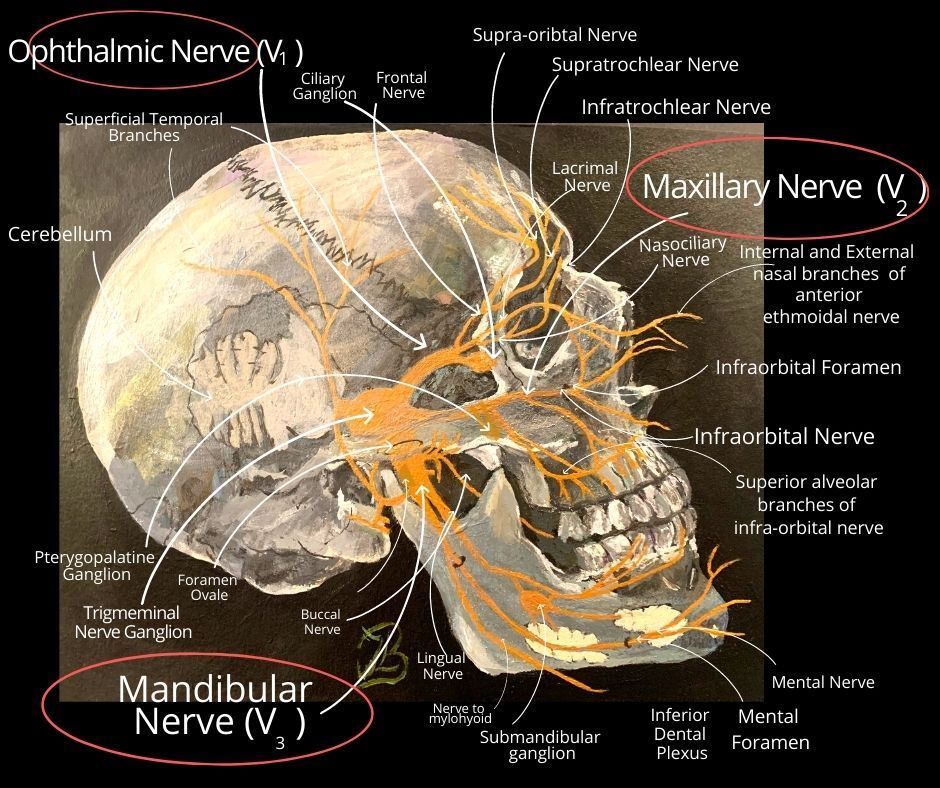
The trigeminal nerve is fascinating for it's unique trait of having four nuclei which sends fibres to its tracts and is associated with three separate main branches distal to the trigeminal ganglion (Figure 1, 2 and 3):
- Ophthalmic (V1):The first branch controls sensation in a person's eye, upper eyelid and forehead.
- Maxillary (V2): The second branch controls sensation in the lower eyelid, cheek, nostril, upper lip and upper gum.
- Mandibular (V3): The third branch controls sensations in the jaw, lower lip, lower gum and some of the muscles used for chewing.
A hyperactive masseteric (jaw-jerk) reflex is commonly seen in dementia and various neurological conditions but has no clear diagnostic significance.
Figure 3 shows the small neural branches of the trigeminal nerve (V); the Infraorbital nerve (ION), Supraorbital nerve (SON), the supratrochlear nerve (ST) and the mental nerve (M).
The Supraorbital Nerve (SON): Is one of two branches of the frontal nerve which itself, is a branch of the ophthalmic nerve (V1). The SON travels anteriorly above the levator palpebrae superioris muscle and exits the orbit via the supraorbital foramen within the superior margin of the orbit (19). The SON then ascends onto the forehead and divides into the medial (SONm) and lateral (SONl) branches of the SON (Figure 3).
The Supratrochlear Nerve (ST): The other branch of the frontal nerve is the supratrochlear nerve which passes above the superior oblique muscle and exits the supratrochlea notch to provide sensory innervation to the forehead and upper eyelid (19) (Figure 3).
The Infraorbital Nerve (ION): A branch of the maxillary nerve (CN V2) that travels through the orbit, enters the infraorbital canal and exits out onto the face via the infraorbital foramen providing skin sensation to the middle of the face (19) (Figure 3).
The ION divides into four main branches; the inferior palpebral (IP), the external nasal (EN), the internal nasal (IN), and the superior labial branches (SLm and SLl) .
The Mental Nerve (M): branches from mandibular nerve (CN V3 ), it emerges from the mental foramen in the mandible and divides into three branches with one branch descending to the skin of the chin via the Mental branch nerve (M). The other two branches ascend to the skin of the lower lip via the lateral (ILl) and medial inferior labial branches (ILm)(19) (Figure 3)
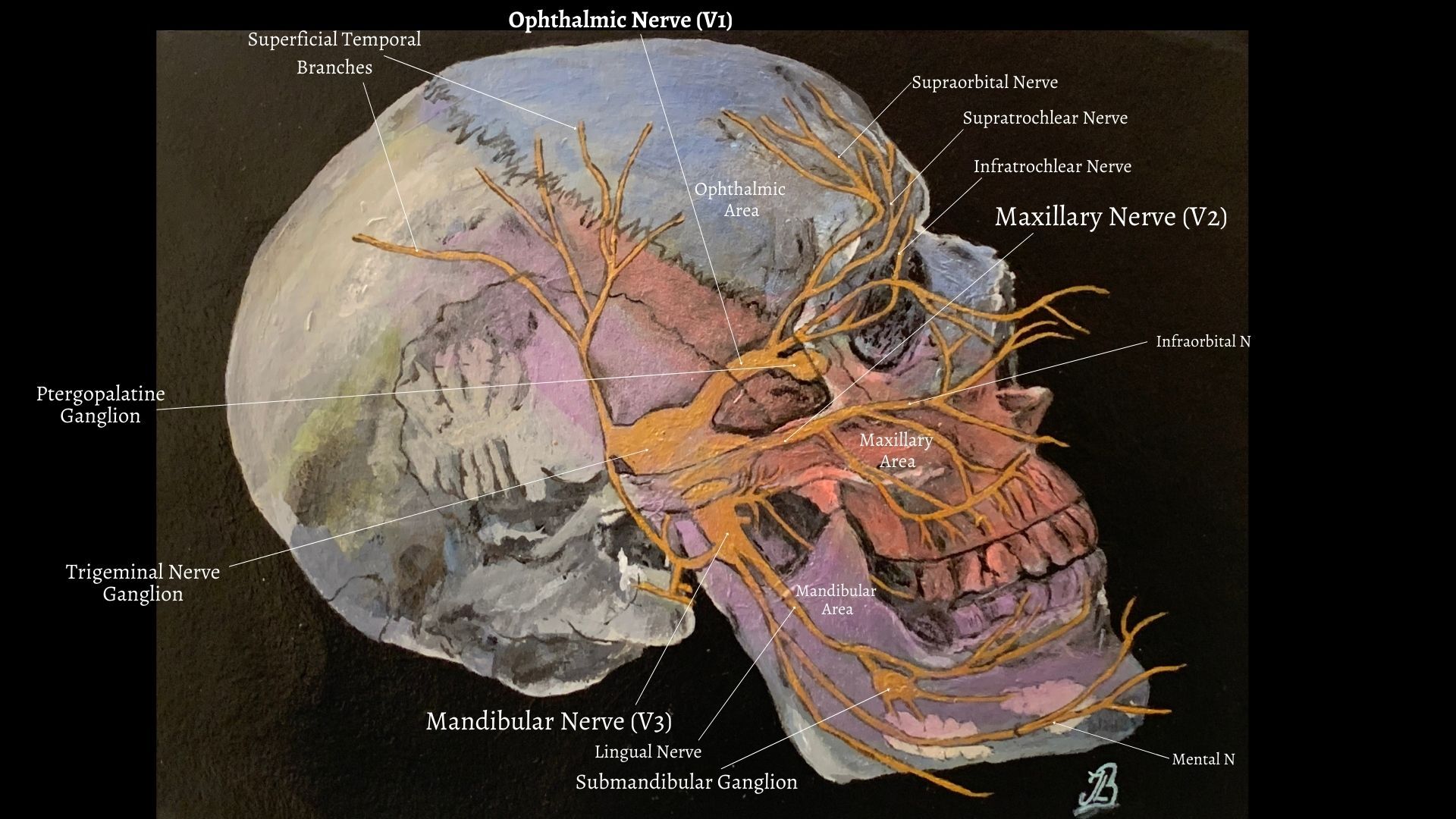
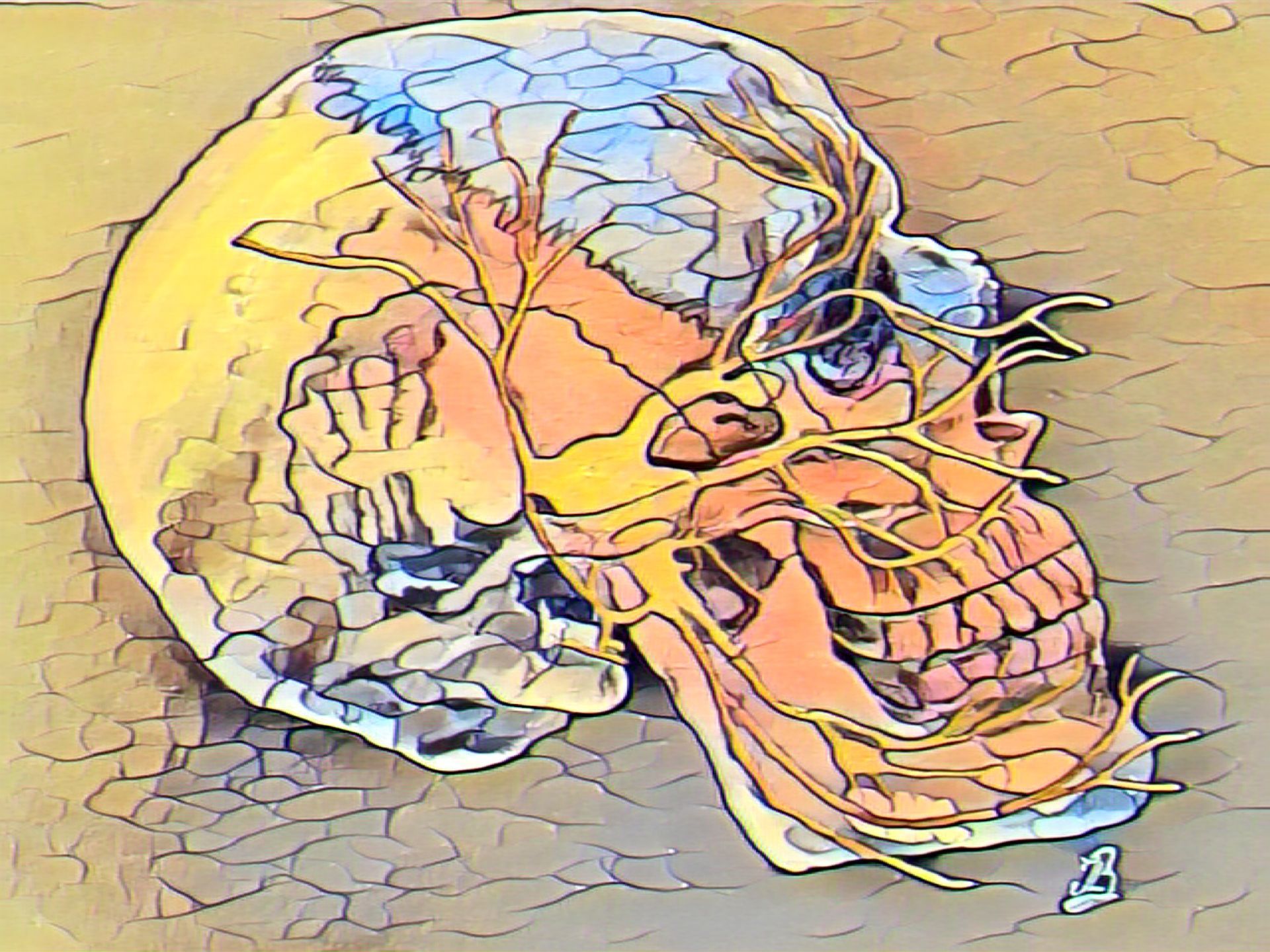
Figure 4 shows how trigeminal nerve divides into three smaller branches after leaving the brain from a side on view. The branches extend to different territories and control sensations throughout the face and join at the trigeminal ganglia which are located within the Meckels cave of the cranial cavity (Figure 4) (19).
Figure 4 shows how each branch provides sensation to particular areas of the face and depending on which branch part of the nerve is irritated, trigeminal neuralgia pain can be felt anywhere in the face. Most commonly, symptoms are felt in the lower part into the jaw region. The intensity of the pain is exceptional with some people reporting it to be more severe than experiencing a heart attack, passing a kidney stone or even giving birth.
Branches V1, V2, and V3 of the trigeminal nerve exit the cranium through the superior orbital fissure, foramen rotundum, and foramen ovale, respectively (2).
Trigeminal Neuropathies: Trigeminal Neuropathy (TNO) Vs Trigeminal Neuralgia (TNA)
Trigeminal neuralgia (TNA) is characterized by brief attacks of lancinating or stabbing sensation like pain, but not cause sensory impairment or motor weakness.
Causes
The International Headache Society (IHS) describes two classifications of TN: classical or primary and symptomatic or secondary (16).
Classical or Primary TN
Classical or primary TN is due to a vascular compression of the trigeminal root by tortuous or aberrant blood vessels (14).
Primary trigeminal neuralgia has been linked to the compression of the trigeminal nerve, typically in the base of the head where the brain meets the spinal cord. This is usually due to contact between a healthy artery or vein and the trigeminal nerve at the base of the brain. This places pressure on the nerve as it enters the brain and causes the nerve to misfire (15, 16).
Accoriding to Gerwin (2020), the vessel most commonly compressing the trigeminal nerve root is the superior cerebellar artery (SCA), as identified by high-resolution magnetic resonance imaging (MRI). The anterior inferior cerebellar artery (AICA), the basilar artery, and an ectatic vertebro-basilar artery have also been implicated in some patients. The trigeminal nerve can also be compressed by veins, particularly the superior petrosal and transverse pontine veins (6).
Symptomatic or Secondary TN
Secondary Trigeminal neuralgia is caused by pressure on the nerve from either a tumor, Multiple sclerosis, a cyst, facial injury or another medical condition that damages the myelin sheaths (16).
Symptomatic TN can be related to cerebello-pontine angle tumours which compress the trigeminal nerve root. Multiple sclerosis (MS) is typically associated with TN (2-4% of patients with TN) (14).
Treatment Options
Non-Surgical Treatments
There are several effective ways to alleviate the pain, including a variety of medications which are generally started at low doses and increased gradually based on patient’s response to the drug (13). Sodium channel blockers of either Carbamazepine or Oxcarbazepine are effective in most TN cases for treating symptoms. However, they can cause possible side effects of dizziness, double vision, drowsiness and nausea. Oxcarbazepine may be preferred for the minor risk of drug interactions and tolerability (14).
Surgery
If medications have proven ineffective in treating TN several surgical procedures may help control the pain, however, microvascular decompression of the trigeminal nerve root is the most effective and long-lasting treatment. Surgical treatment is divided into two categories: 1) open cranial surgery or 2) lesioning procedures. In general, open surgery is performed for patients found to have pressure on the trigeminal nerve from a nearby blood vessel, which can be diagnosed with imaging of the brain, such as a special MRI. This surgery is thought to take away the underlying problem causing the TN. In contrast, lesioning procedures include interventions that injure the trigeminal nerve on purpose, in order to prevent the nerve from delivering pain to the face. The effects of lesioning may be shorter lasting and in some cases may result in numbness to the face.
How Might Physical Therapy Help?
Acupuncture - Case Study
A previous case study by Sert et al., (2009) reported that acupuncture treatment helped relieve their symptoms after having received 5 treatment sessions. A 66 year old lady who suffered from chronic TN pain on the left side of her face for over 25 years found that acupuncture helped relieve her symptoms completely despite trying primary care intervention methods first. The primary care methods included medication (carbamazepine, gabapentin and valproic acid), nerve block and radiofrequency rhizotomy of the infraorbital branch of the trigeminal nerve (16).
However, research has concluded that although acupuncture may have some positive effects on Trigeminal Neuralgia, the level of evidence is low or very low and a firm conclusion can not yet be drawn on the efficacy of acupuncture for Trigeminal Neuralgia (16).
Deep Tissue Massage & Acupuncture - Case Study
Another case who suffered from TN was studied by Omar and Bakar (2020) who found that acupuncture with massage therapy had significantly improved their symptoms after four treatment sessions. The massage applied involved using deep pressure along the distribution of the trigeminal nerve around the regions of the ear, maxilla, mandibular, and forehead. The massage aimed to stimulate the nerve by repeatedly stroking along the distribution of the V2 trigeminal nerve. Dry needling was executed at five location points, namely the temporalis muscle, the junction of the temporo-mandibular joint and along the lower end of the maxillary bone including masseter muscle (13).
Spinal manipulation and Chiropractic Care - Case Study
Another case study who received chiropractic care and suffered from chronic TN pain was written by Rodine and Aker (2010). In this particular case, there was evidence to suggest that there were three sources of pathology contributing towards the individual's pain including; neck pain caused by degenerative disc disease (DDD), temparomandibular joint (TMJ) syndrome and trigeminal neuralgia (16). The chiropractic practitioner observed the relief of symptoms by performing ultrasound electrotherapy, manual therapy of manipulation and mobilisation, soft tissue therapy techniques and home exercises.
Osteopathic Treatment & Cranial Osteopathy
Some individuals might find relief from osteopathic treatment application to the cranium, in particular the cranial base with myofascial trigger points to the masseter and temporalis muscles (2).
References
- Birnbaum G and Iverson JDalfampridine may activate latent trigeminal neuralgia in patients with multiple sclerosis.Neurology 2014;83(18): 1610-161
- Campbell, S., M., Winkelmann, R. R., Walkowski, S. (2014) Osteopathic Manipulative Treatment Novel Application to Dermatological Disease, Clinical Aesthetic, 5; 10: 24-32.
- Crevier-Sorbo, G., Brock, A., Rolston, J. D. (2019) Trigeminal neuralgia plus hemifacial spasm caused by a dilated artery: a case of painful tic convulsif syndrome, Lancet, 394, e36.
- Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. (2008) AAN‐EFNS guidelines on trigeminal neuralgia management. European journal of neurology; 15 (10): 1013-28.
- Dalessio D, J. (1982) Trigeminal neuralgia. A practical approach to treatment. Drugs; 24 (3): 248-55. Physiotherapy/Physical Therapy. Available from: Physiotherapy / Physical Therapy.
- Gerwin, R. (2020) Chronic Facial Pain: Trigeminal Neuralgia, Persistent Idiopathic Facial Pain, and Myofascial Pain Syndrome—An Evidence-Based Narrative Review and Etiological Hypothesis, MDPI, 17, 7012.
- Headache Classification Committee of the International Headache Society (IHS) (2013) The International Classification of Headache Disorders. Cephalalgia; 33:629–808. 3rd edn.
- Kataria, S., Ahmed, Z., Ali, U., Ahmad, S., Awais, A. (2020) Trigeminal Neuralgia Induced Headache: A Case Report and Literature Review, Cureus, 12; 7: 1-4.
- Khanal, D., Khatri, S. M., Anap, D. (2014) Is there Any Role of Physiotherapy in Fothergill's Disease. Journal of Yoga & Physical Therapy. 1; 4 (2): 1.
- Kim, J.I., Kim, H.J., Lee, J.J., Jun, J.H., Choi, T-Y., Lee, M. S. (2018) Acupuncture for the treatment of trigeminal neuralgia A protocol for the systematic review of randomized controlled trials, Medicine, 97; 11: 1-3.
- Liu, G. T. (2001) Neuro-ophthalmology: Diagnosis and Management: The Trigeminal Nerve and Its Central Connections; Chapter 25: pp. 1233-1268.
- Liu, H., Li, X-W., Du, J. (2019) Acupuncture Treatment on Idiopathic Trigeminal Neuralgia, Study Protocol Systemic Review, Medicine, 98; 4: 1-5.
- Longo, D. L., et al., (2017) eds. Trigeminal neuralgia, Bell's palsy, and other cranial nerve disorders. In: Harrison's Principles of Internal Medicine. 19th ed. New York, N.Y.: McGraw-Hill Education; 2015. https://accessmedicine.mhmedical.com. Accessed June 5.
- Omar, W. A. W., Bakar, N. L. A. (2020) Improvement of trigeminal neuralgia after massage therapy and dry needling, Malaysian Journal of Medicine and Health Sciences;16 (102): 81-83.
- Maarbjerg, S., Stefano, G. D., Bendsten, L., Cruccu, G. (2017) Trigeminal Neuralgia; Diagnosis and Treatment, Cephalalgia, International Headache Society, 37, 7; 648-657.
- Reeta, Kumar U, Kumar V, Alam M, Islami D, Lal W et al (2016). A Survey to Observe the Commonly Used Treatment Protocol for Trigeminal Neuralgia by Physiotherapist. International Journal of Physiotherapy; 3 (5): 643-646.
- Rodine, R. J., Aker, P. (2010) Trigeminal Neuralgia and Chiropractic Care: A Case Report, JCCA, 54;3: 177-186.
- Sert, H., Usta, B., Musla, B., Gozdemir, M. (2009) Successful Treatment of a Resistance Trigeminal Neuralgia Patient By Acupuncture, Clinics, 64(12): 1225–1226.
- Smith, J. H., Cutrer, M. F., (2011) Numbness Matters: A Clinical Review of Trigeminal Neuropathy, Cephalalgia, International Headache Society; 0 (0) 1–14.
- Truini. A (2015), Trigeminal Neuralgia, Journal of Headache and Pain, 16; A42.
- Trigeminal neuralgia. Available from: https://www.physio.co.uk/what-we-treat/chronic-pain-fatigue/trigeminal-neuralgia.php (Accessed on 2nd October, 2020).
- Wikipedia (2022) [online] https://en.wikipedia.org/wiki/Mental_nerve#:~:text=The%20mental%20nerve%20is%20a%20branch%20of%20the.... (last visited 07/02/2022).