Nerve Entrapment, Injury and Neuropathy; The Radial Nerve
- by Joanna Blair
- •
- 05 Sept, 2021
- •
Anatomy & Treatment Options
The radial nerve's anatomical position with relation to it's close proximity to the humeral shaft of the humerus makes it particularly vulnerable should a fracture occur. Injuries to the radial nerve may occur at any point along the nerve’s route and radial nerve palsy can result from a variety of aetiologies.
Although most common to injury, a radial nerve injury is the least debilitating for upper limb nerve injuries and treatment is often non-operative.
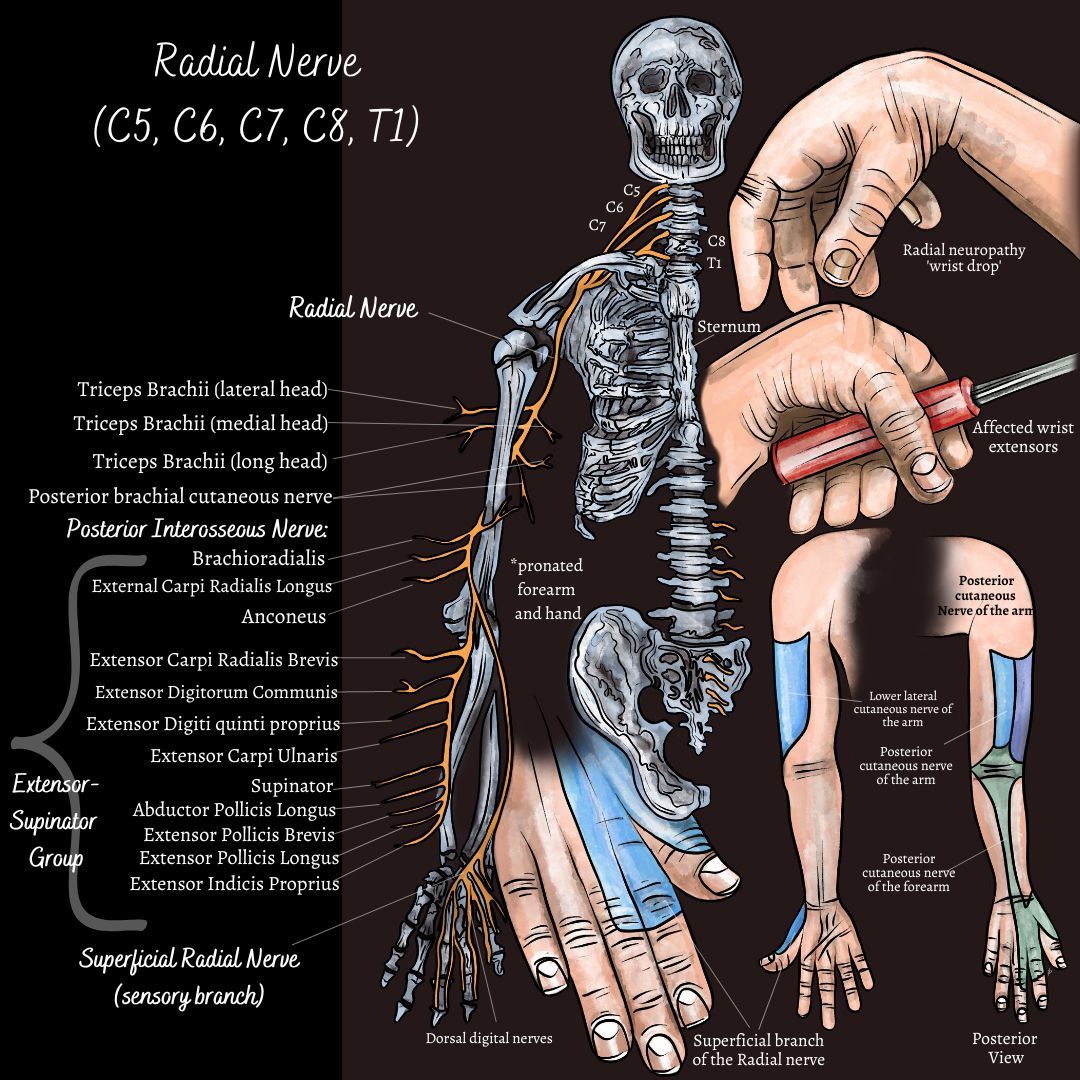
Sensory Provision
Lower lateral cutaneous nerve of the arm: from the inferior aspect of the deltoid insertion of the humerus and innervates the lateral aspect of the middle to lower arm.
Posterior cutaneous nerve of the arm: innervation to the posterior surface of the arm.
Posterior cutaneous nerve of the forearm: innervates a strip of skin down the middle aspect of the posterior forearm.
Superficial branch of the radial nerve: Innervating the dorsal surface of the lateral two and half digits of the dorsum hand, although some sources state the lateral three and half digits.
Anatomy
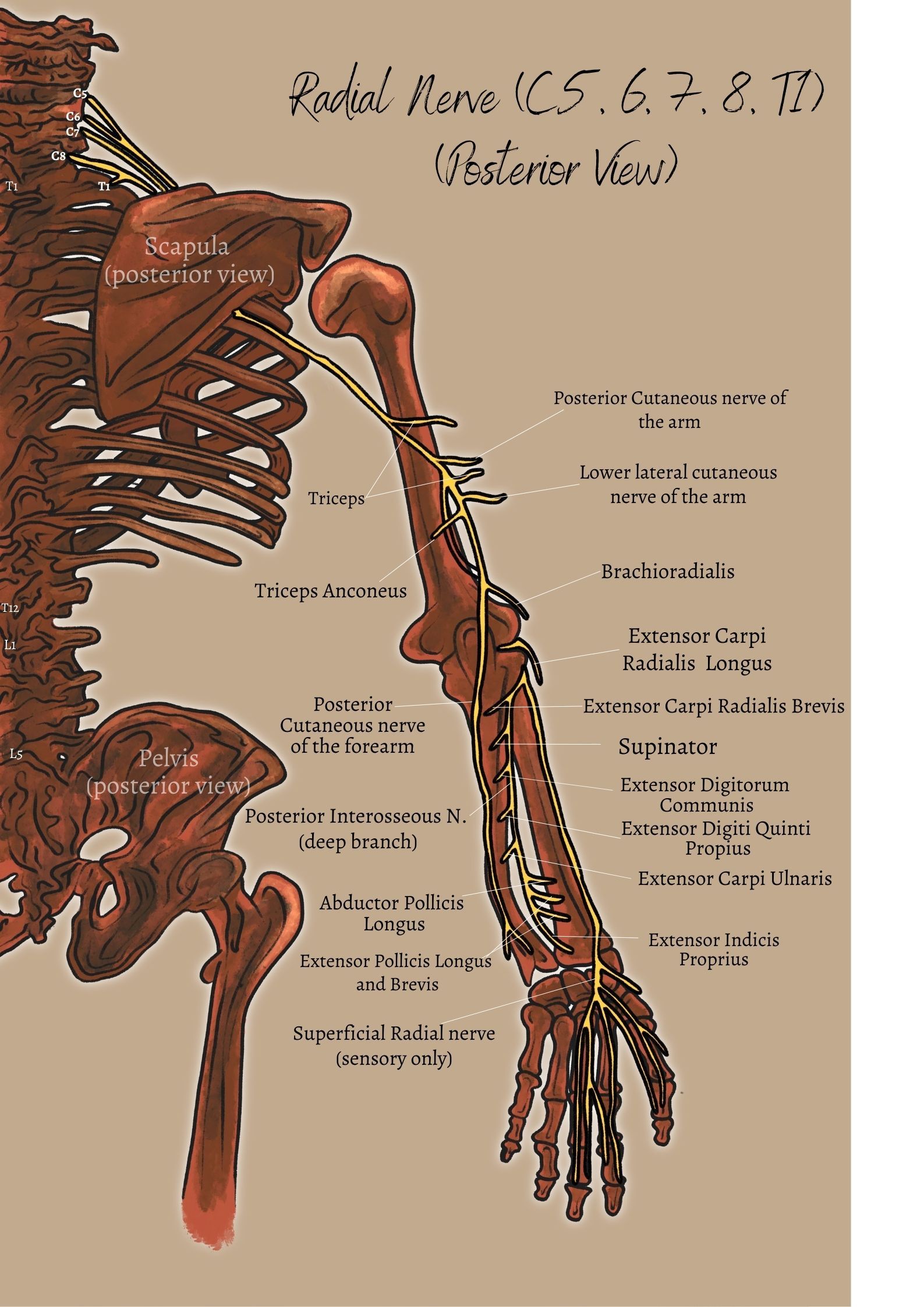
The radial nerve originates as the terminal branch of the posterior cord of the brachial plexus at nerve roots C5 to C8 and T1. The nerve arises from the posterior aspect of the axilla and descends along the posterior surface of the humerus (figure 1) before passing through the cubital fossa and terminating in the posterior compartment of the forearm into two main branches; the sensory and motor branch.
The radial nerve gives off three sensory branches and innervates three heads of the triceps muscle and the small anconeus muscle. The nerve then snakes its way down the humerus in the spiral groove and gives muscular branches to the following muscles beforebifurcating into superficial (sensory) and deep (motor) branch (figure 2):
- Brachioradialis (beneath)
- Ext. Carpi Radialis
- Supinator
This part of the radial nerve travels down the forearm over the radial bone and over the extensor tendons to the thumb and supplies the majority of the dorsal surface of the hand (6).
The Posterior Interosseous Nerve
This nerve is a motor branch that runs along the lower neck of the humerus before entering the extensor compartment and piercing through the supinator muscle where it supplies the remaining extensors of the wrist, thumb and finger.
The Posterior Antebrachial Cutaneous Nerve
Upon entering the cubital region and before its division, the radial nerve provides the posterior antebrachial cutaneous nerve which is also a sensory branch and innervates the strip of skin down the middle of the posterior forearm, as mentioned above (4).
The Deep Branch - the "motor branch" of the Radial Nerve
Provides motor innervation (i.e. innervating muscles to produce motion) to the posterior compartment of the forearm.
Injury, Entrapment Sights and Clinical Examination of the Radial Nerve
Entrapment of the radial nerve is uncommon but the most frequent location, should it happen, may occur at the proximal forearm or in proximity to the supinator involving the posterior interosseous nerve branch (2).
Radial Tunnel Syndrome (RTS)
The radial tunnel extends from the radial head to the inferior border of the supinator muscle and the boundaries consist of the supinator, extensor carpi radialis longus and brevis and the brachioradialis muscles.
The injury is more prevalent in women between ages 30 to 50 years old and mainly occurs via intermittent compression on the radial nerve from the radial head to the inferior border of the supinator muscle without notable extensor muscle weakness (2, 3, 4).
Entrapment of the radial nerve may occur as a result of overuse or repetitive actions and exercise involving pronation or supination (e.g. frequent use of a screw driver), direct trauma, fractures, or involve the posterior interosseous nerve due to it being situated at the level of the radiocapitellar joint (between the radial head and the lateral condyle of the humerus) (2, 4) (Figure 3).
Four other Sites for Radial Nerve Entrapment:
- Fibrous bands around the radial head.
- Recurrent Radial vessels.
- Arcade of Frohse.
- Tendinous margin of the extensor carpi radialis brevis.
Overall, the radial nerve is most vulnerable to injury at the mid-humeral level.
Radial Palsy & Wrist Drop (Figure 3.)
The main clinical feature of a radial nerve injury is wrist drop as the flexor tone overpowers the nonfunctional wrist extensors and the hand is pulled into a flexed position. The wrist might be able to be passively extended into place, but the patient is unable to actively maintain the position. Extension of the the fingers at the metacarpophalangeal joints and the inability to extend or abduct the thumb can also be lost, thus causing the patient the inability to open the hand prior to initiating grasp (2, 4).
As Figure 3 demonstrates, occupational performance can be affected as the absence of oppenens pollicis may reduce muscle power whilst grasping a hammer or screw driver handle or whilst writing with a pen.
The Spiral Groove & 'Saturday Night Palsy'
External compression or trauma via fracture along the shaft of the humerus at the spiral groove can also cause radial neuropathy and be attributed from immobilisatoin of the arm. A common cause can be from patients falling asleep with their arm draped over a chair (usually after intoxication) and is classically known as "Saturday Night Palsy" (2). Clinically, patients present with wrist drop, weakness of finger extension and dysesthesia along the distribution of the superficial radial nerve. Often, supination is weakened but elbow extension is spared as the branches to the triceps originate before the spiral groove.
Radial Neuropathy and the Use of Crutches
External compression from inadequate use of crutshces can also cause vulnerability to the radial nerve which can cause weakness in elbow extension and sensory loss within the proximal cutaneous branches. This can entrap the posterior interosseous branch of the radial nerve within the supinator muscle under the arcade of Frohse along with the patient showing signs of wrist drop and weakness in supination (6). Clinical signs for this might involve radial deviation as the patient attempts to extend the wrist and sensory dysesthesia.
Osteopathy & Possible Treatment Management
Radial Nerve Flossing Exercise:
Osteopathic treatment may consist of gentle soft tissue massage applied to the local and relevant muscles along with articulation to neighbouring joints to areas such as the neck, mid back and shoulders with the aim of reducing muscle tightness, tissue swelling and providing physical space for the trapped nerve. Other treatment modalities might also be offered such as medical acupuncture to reducing muscle spasm, and trigger points along with passive and active stretching, muscle energy techniques, electrotherapy, home exercises such as a nerve 'flossing' home programme and postural adaptations and lifestyle advice.
If the problem is severe or not resolving, a Magnetic Resonance Imaging (MRI) scan is usually referred to establish the cause of the neuropathy and the result can help the practitioner know whether a medical referral for a surgical opinion or rheumatologist is necessary.
References
2. Buchanan, B. K., Varacallo, M. (2018) Radial Nerve Entrapment, StatPearls, NCBI Bookshelf,
3. Colditz, J. C. (1987) Splinting for Radial Nerve Palsy, Journal of Hand Therapy, 18-27.
4. Kenhub (2020), the Radial Nerve, Available From: https://www.kenhub.com/en/library/anatomy/radial-nerve [online] last viewed 2/09/2021.
5. Ljungquist, K. L., Martineau, P., Allan, C. (2015) Radial Nerve Injuries, ASSH, Elsevier, 40: 166-171.
6. McNamara, B. (2003) Clinical Anatomy of the Radial Nerve, ACNR, 3; 3: 28-29.