Spinal Degenerative Disc Disease
- by Joanna Blair
- •
- 28 Jan, 2024
- •

Condition, Anatomy and Management
Degenerative disc disease (DDD) is not a disease but a condition that usually occurs over time from ageing. The degeneration of intervertebral disc tissue starts earlier than the degeneration of other muscular and skeletal tissue (9). Interestingly, degeneration is likely to start almost ten years earlier in men than women, but women with disc degeneration are likely to be more susceptible to the effects e.g. malalignment and instability (9).
Statistics show that approximately 20% of individuals within their teenage years may show signs of mild disc degeneration and approximately 10% of individuals show severe disc degeneration in their 50's (9). The percentage rate of severe degenerative disc disease climbs to approximately 60% in 70-year olds (9). These statistics show that maintaining the health of our spine as we age is extremely important.
The Intervertebral Disc
The intervertebral discs make up one fourth of the spinal column and can be described as pads of fibrocartilage-based structures found between each vertebral body within the spine (3). They are important for the following reasons:
- Connecting the vertebrae and providing spinal mobility for the movements of bending and rotating (1).
- Providing support, flexibility and minor load-sharing (3).
- Shock absorption between vertebrae.
- Help mechanical stresses to be transmitted throughout the spine during movement from the lower limbs into the neck and skull (1).
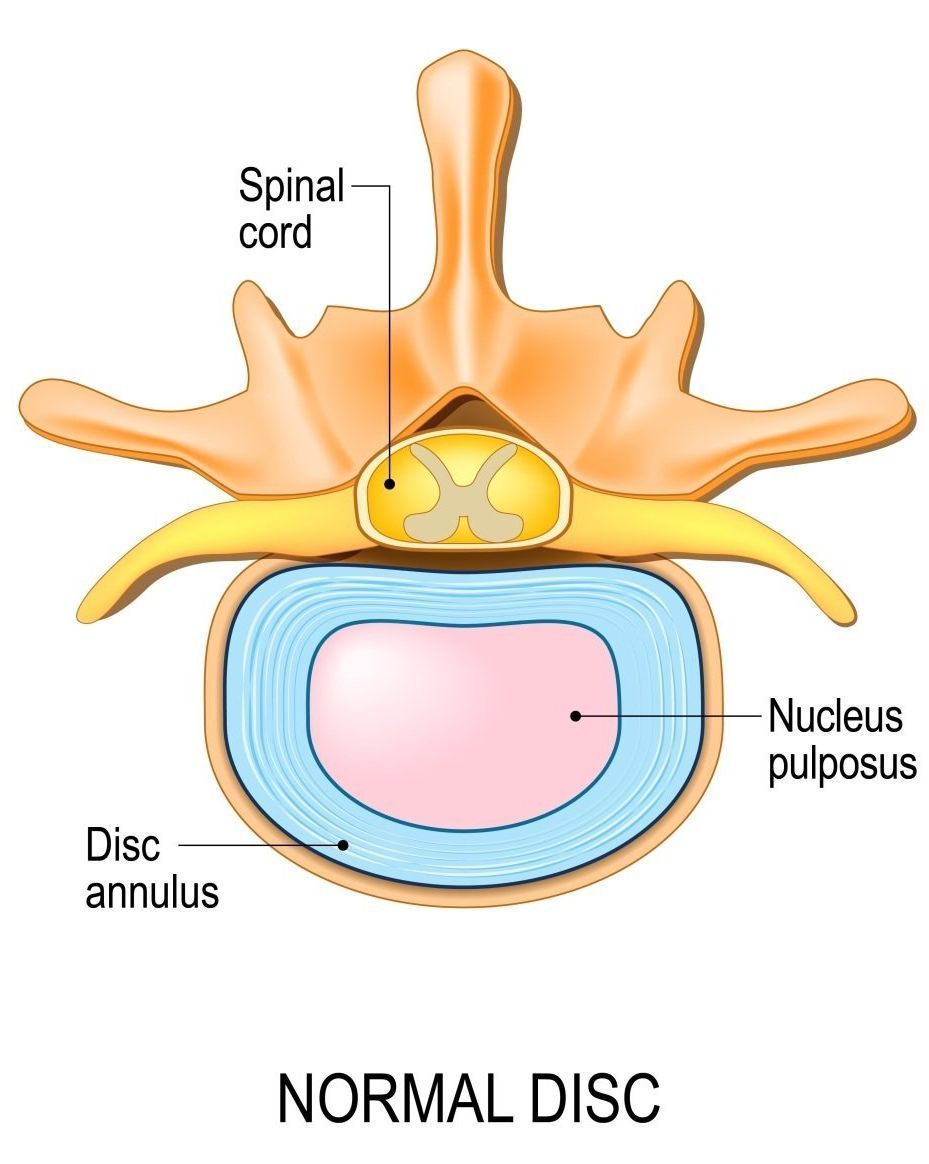
The intervertebral disc is composed of two parts; an outer strong ring called the annulus fibrosus that surrounds a soft gel-like inner substance called the nucleus pulposus consisting of 80% to 85% of water in normal/ non pathological cases (1).
Disc Herniation/ Prolapse
Disc herniation results when there is disruption to the disc structure, mainly from tearing of the annulus fibrosis to create a protrusion of the inner nucleus pulposus against the annulus fibrosis. This creates pressure to the spinal cord or nerve root resulting to radiating pain and create specific locations of weakness within the lower back and limbs. Over 90% of herniated discs appear at segments L4/L5 and L5/ S1 (4). This compression can produce radiculopathy or referred neurological pain, muscular weakness, altered sensations (paresthesia) and the difficulty of controlling specific muscle movements especially within the the back of the leg and at front of the foot (4).
There are several causes for annual tears including (10):
Degenerative Disc Disease: The spinal discs degenerate via wear and tear to cause fluid loss and a reduction in disc height, leading to a loss of spinal flexibility and increase the risk for disc tear.
Bone Spurs: Bone spurs are boney nodules that form within the endplates of the vertebra as a result of inflammation and can cause annular tears if they extend into the disc space.
Trauma: Traumatic injuries such as sports collisions, car accidents and falls can cause damage to a spinal disc.
Overuse: Repetitive, heavy lifting and occupations that place chronic strains on the back e.g. sports, nursing, or trading jobs that require heavy lifting can cause annular tears.
Genetics: Genes often determine the strength and quality of muscle collagen which is otherwise the substance that makes up the annulus. Poor cartilage production or inferior collagen can increase risk of annular tears.
It is interesting to note that the thickness and intensity of different parts of the annulus fibrosis (AF) is different. The posterior aspect of the lumbar intervertebral disc is thinner and there are no collagen fibres interwoven which lowers the tissue intensity and explains why disc herniation often occurs at the back of the intervertebral disc (13).
'Degenerative Disc Disease'
Most intervertebral disc degenerations are asymptomatic with that patients can have the problem diagnosed from scans but not experience pain. The absence of a diagnosis via relevant medical imaging via i.e. Magnetic Resonance Imaging (MRI) can prove difficult for physical therapy practitioners to manage.
Back pain symptoms related to intervertebral disc degeneration are caused by pathological changes within the disc known as 'disc desiccation' or the 'drying out' of the water content within a disc. The condition causes the following:
- Fibrosis; a thickening or scarring of tissue.
- Disc narrowing causing a reduction of disc height and/ or width.
- The annulus to bulge, fissure or undergo degeneration.
- Arthritis within the vertebrae.
The biochemistry of disc degeneration indicates that enzymatic activity contributes to this disorder by causing increased fragmentation of collagen, proteoglycan and fibronectin within the disc (13). Several families of enzymes are capable of breaking down the various matrix molecules within the disc, including cathepsins, MMPs and aggrecanases (13).
The most significant biochemical change to occur in disc degeneration is a loss of proteoglycan protein and collagen Type II. Aggrecan is the major proteoglycan of the disc and responsible for maintaining tissue hydration through the osmotic pressure provided by chondroitin and keratan sulphate chains (13). The proteoglycan and water content of the nucleus is greater than in the annulus (13).
Proteoglycan loss reduces the capacity of tissues binding to water leading to a loss of hydration within the disc and decreases intervertebral joint load-bearing (13). Proteoglycan loss causes the osmotic pressure of the disc to fall and the disc less able to maintain hydration under load (13). Degenerative discs have a lower water content than other age-matched discs within the spine which accelerates the rate of fluid loss, reduces disc height and creates a higher risk for discs to bulge (13).
Loss of proteoglycan and extracellular matrix disorganisation have an important mechanical effect within the disc with that the subsequent loss of hydration means that the degenerated disc is no longer able to behave hydrostatically under load (12). Loading may lead to inappropriate stress concentrations along the end-plate or within the annulus (12).
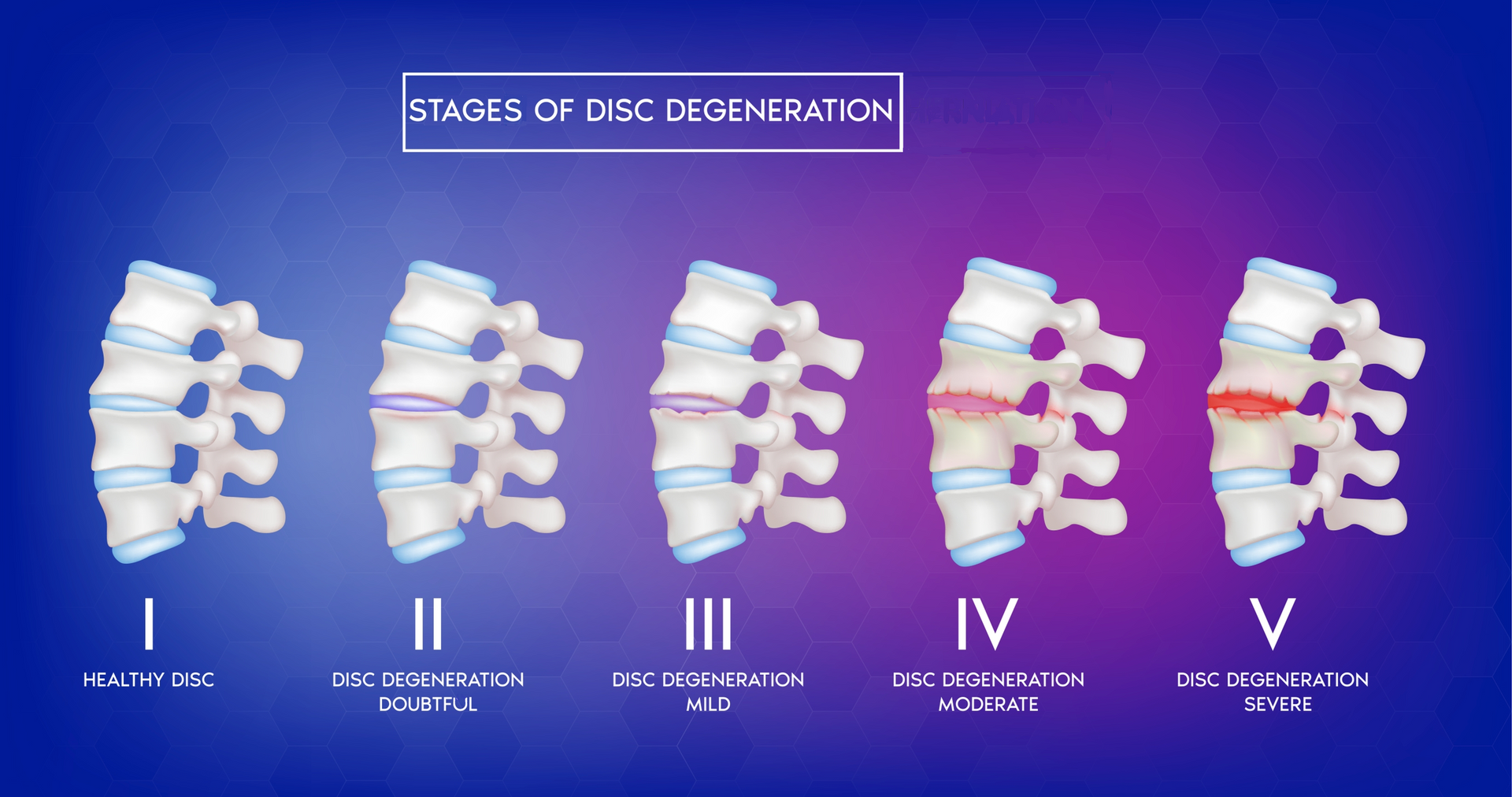
The Pfirrmann Grading System (4):
The Pfirrmann Grading System is a five graded system for practitioners to use for the assessment of lumbar disc degeneration with subtle changes seen within grades I-III, a moderately reduced disc height might be seen in grade IV and a collapsed disc space observed in grade V (4).
Griffith et al., (2017) encourages the idea for health practitioners to use a modified eight graded Pfirrmann system for the assessment of disc degeneration within the elderly spine. This can help discriminate the severity of disc degeneration in more depth and detail. Grade I corresponds to having no disc degeneration, while Grade 8 represents a severe or 'end-stage' degeneration. A grading system in Table 1 of their study was devised and showed how the disc space height is more visibly lost between Grades, 6, 7, and 8 and is broadly classified as 'mild', 'moderate', to 'severe' (loss of disc space height) between these grades (6).
Can This Create Nerve Irritation?
Progression can cause the disc to bulge and create pressure and irritation to neighbouring spinal nerves. This can lead to individuals experiencing tingling (paraethesia) into the limbs of the body such as the arms and fingers for if the region is affecting areas of the neck or buttock, thigh and/ or toes for if occurring within the lower back (12).
Recent studies have shown that atrophy and muscle weakening can gives rise to disc degeneration and cause pain and instability within the spine. The ageing process for degenerative disc disease can cause mobility issues and a reduced spinal shock-absorbing capability. Research has found disc degeneration and lumbar multifidus muscle atrophy to be commonly correlated, particularly at spinal disc levels L3-L4 (5).
Possible Causes
In most cases, disc desiccation happens from ageing. Other reasons include:
- Trauma such as accidents
- Sudden weight loss
- Hereditary cause
Smoking creates various negative effects to the musculoskeletal system by lengthening the healing time of tissues post injury or trauma. Smoking will hinder disc healing as tissue oxygenation is reduced and cellular metabolism is disrupted.
Tissue hydration is compromised; the production rate of proteoglycans is reduced which otherwise provides hydration and swelling pressure to the disc tissue to help withstand compressional forces (14).
Nicotine causes elevated levels of pro-inflammatory cytokine protein TNF-α which prolongs pain states (7). Because smoking or vaping increase and hinder tissue healing and elevate pain levels, orthopaedic surgeons are reluctant to operate.
Diagnosis
Intervertebral discs at some certain segmental levels undergo more degeneration than others which implies that mechanical stress plays a role in disc degeneration (8). The occurrence of dessicated or dried up discs mostly appear within the lower back or lumbar discs, in particular the lower three to four discs i.e. between L3-L4, L4-L5, L5-S1 and S1 (2).
However, any part of the spine can develop disc degeneration (11). As Griffith et al., (2007) highlight, Magnetic Resonance Imaging (MRI) is the most widely used method for assessing intervertebral disc degeneration. Based on proton density, water content, and chemical environment, an MRI depicts disc hydration and morphology (6).
In osteopathy, the somatic dysfunction (SD) addresses abnormal posture and biomechanics (the way we move). As Kessler et al., (2021) highlight, this can start a pathological cascade of degenerative disc disease and annular tearing as this can limit active range of motion and cause asymmetric loading within neighbouring joints.
Treatment and Management

Therapies are designed to reduce pain rather than repair degenerated discs (13). Treatments are mainly conservative and palliative ranging from analgesia, corticosteroid injections, local anaesthetic and manipulation therapies all with the main aim of returning patients to work (13).
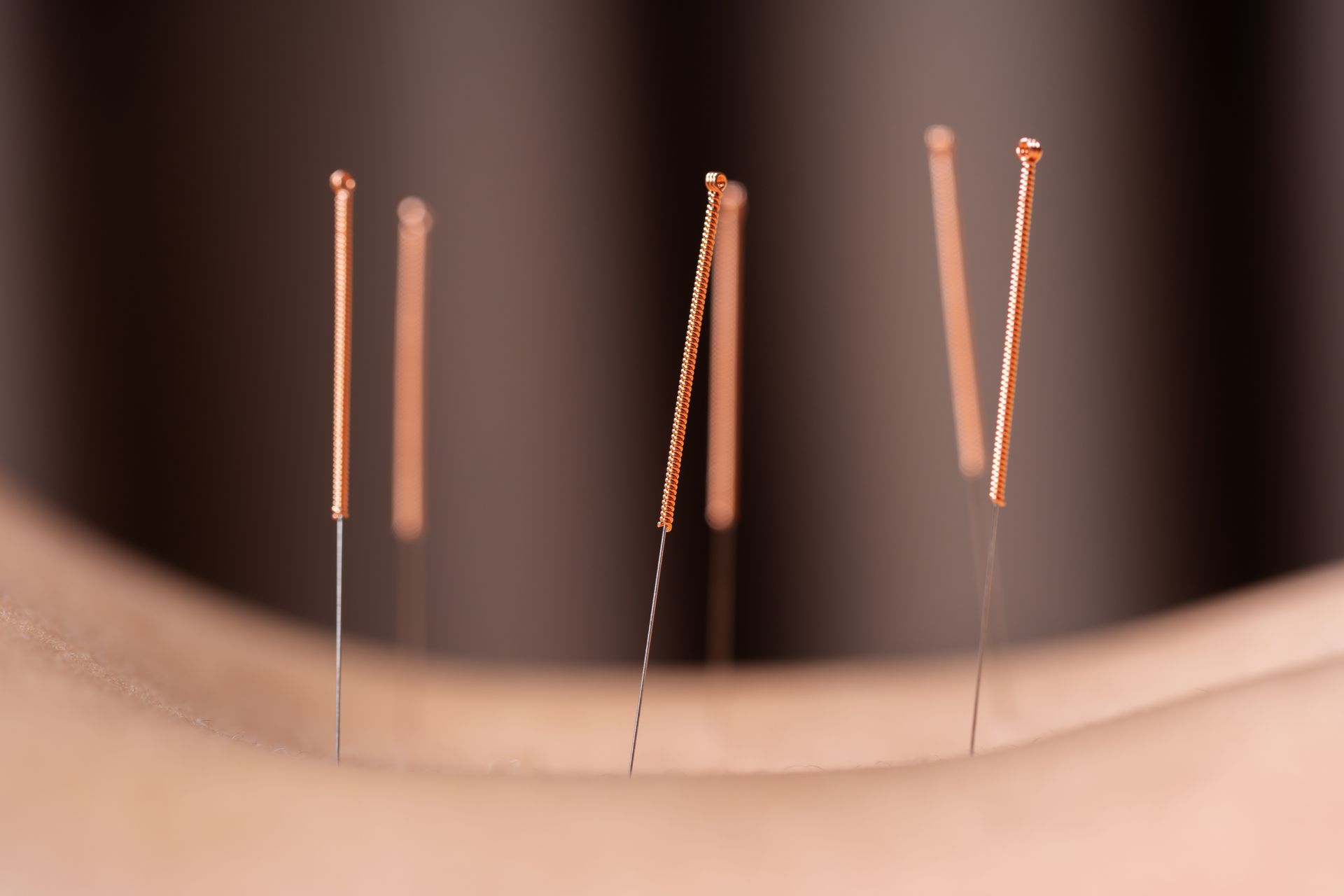
Physical therapy is the preferred method for treating individuals with DDD and therapists mainly aim to strengthen neighbouring muscles around the affected joints. Before 'hands on' Spinal Manipulation Therapy (SMT)' can be considered as a treatment option, patients will need to be screened for possible serious pathology.
Osteopathy
Various physical therapy modalities might be applied. Osteopathic treatment may include gentle hands on joint mobility and articulation treatment techniques of the spine and surrounding tissues. The of use of hands on stretching and gentle joint motion mobilisation techniques might be applied along with exercise programs and electrical stimulation therapy such as interferential therapy, remedial massage techniques and modified lifestyle advise e.g. related to weight loss and smoking cessation.
Dynamic Lumbar Stabilization Program (DLSP)
The study by Faur et al., (2019) found that the percentage of lumbar multifidus muscle atrophy is particulalry higher within the lower spinal levels L5 and S1. They concluded a low correlation and significant association between the grade of lumbar disc degeneration and the degree of lumbar multifidus muscle fatty atrophy. They discovered a higher fatty atrophy score in women and a greater incidence of disc degeneration in men (4).
Spinal Exercise Example:
Exercise Prescription
Exercises aims to improve the coordination between the abdominal and back muscles. The above exercise aims to help improve range of motion of the hips and knees, reduce stiffness within the spine and improving the body's mobility to roll to one side whilst in bed.
Motion and strength training will help increase the strength and stability of muscles within the pelvic floor and for those that support the spine and pelvis. Stabilisation exercises increase the body's capacity to resist higher loads in the degenerative discs and reduce injury as muscular tissue reduces at a rate of 1 kg per year after the age of 40 and replaced by fatty tissue (1).
Training exercises performed one to three times per week reduces pain and should be continued once pain has subsided and patients are able to return to their jobs/hobbies or activities and are able to cease the use of analgesics (5). The Williams method involves stretching the back extensor muscles and strengthening abdominal muscles to relieve pressure placed on the lumbar intervertebral discs (5).
Cell Based Therapies
Experiments have been conducted to demonstrate the potential use of of cell-based therapies, however, several barriers prevent the use of these treatments clinically.
The aim of these therapies is to achieve cellular repair of the degenerated disc matrix and one approach has been to stimulate the disc cells to produce more matrix with the use of growth factors which can increase the rate of matrix synthesis by five fold (13). In contrast, cytokines lead to matrix loss as they inhibit matrix synthesis by stimulating the production of agents that encourage tissue breakdown.
However, the injection of growth factors or 'cytokine inhibitors' has not been successful as their effectiveness in the disc is short-lived.
Genetherapy is also being investigated with the aim of maintaining high levels of relevant growth factors or inhibitors within the disc tissue. In this form of therapy, the gene of interest i.e. the one responsible for producing a growth factor such as transforming growth factor-β or inhibiting interleukin-1, is introduced into target cells which then produce relevant proteins (13).
However, this therapy is still not successful for clinical use. The delivery of the genes into human disc cells still remains to be a problem along with an improved understanding for the pathogenesis of degeneration within tissues for the correct choice of therapeutic genes to be applied (13). In addition, the cell density within a normal human disc is low and many of the cells in degenerate discs are dead, thus stimulation of the remaining 'living' cells may be insufficient to repair the extracellular matrix (13).
Nevertheless, when discoverd, this one day could be the future for treating the degenerative disc.
Surgery
Surgical intervention should be reserved for those with either neurologic deficits, degenerative spondylolisthesis, or pain limiting daily functions (4) . Operative intervention of the lumbar spine include discectomy with fusion, total disc replacement or by immobilisation of the affected vertebrae (4). Surgery is offered only to one in every 2000 back pain episodes in the UK; the incidence of surgical treatment is five times higher in the USA (12).
References
1. Alomari, R., Corso, J. J., Chaudhary, V. Dhillon, G. (2009) Dessiccation Diagnosis in Lumbar Discs From Clinical MRI with a Probabilistic Model, Research Gate, https://www.researchgate.net/publication/221624161_Desiccation_Diagnosis_in_Lumbar_Discs_from_Clinic... [online].
2. Brzuszkiewicz-Kuzmicka, G., Szczegielniak, J., Baczkowicz. (2018) Age related changes in shock absorption capacity of the human spinal column, 13: 987-993.
3. Donnally, C. J., Hanna, A., Varacallo, M. (2023) Lumbar Degenerative Disk Disease, StatPearls Publishing LLC [Online], Last visited 12/01/2024.
4. Faur, C., Patrascu, J. M., Haragus, H., Anglitoiu, B. (2019) Correlation Between Multifidus Fatty Atrophy and Lumbar Disc Degeneration in Low Back Pain, BMC Musculoskeletal Disorders, 20; 414: 1-6.
5. Gąsiorowski, A., Zagórski. J. (2013) Strength training in the treatment of degeneration of lumbar section of vertebral column, Annals of Agricultural and Environmental Medicine, Vol 20; 2: 203–205.
6. Griffith, J. F., Wang, Y-X. J., Antonio, G. E., Choi, K. C., Yu, A., Abuja, A. T., Leung, P. C. (2007) Modified Pfirrmann Grading System for Lumbar Intervertebral Disc Degeneration, Spine, 32; 24: pp E708 –E712.
7. Hawkins, J. L., Denson, J. E., Miley, D. R., Durham, P. L. (2018) Nicotine Stimulates Expression of Proteins Implicated In Peripheral and Central Sensitisation, Neuroscience PMC, 290: 115-125.
8. Kessler, R., Haase, C. Dean, D. (2021) An Osteopathic Approach to Patients with Degenerative and Herniated Discs, The AAO Journal, 31; 2: 35-41.
9. Kos, N., Gradisnik, L., Velnar, R. (2019) A Brief Review of the Degenerative Intervertebral Disc Disease, 73; 6: 421-424.
10. Lee, B. H., Moon, S-H., Suk, K-S., Kim, H-S., Yang, J-H., Lee, H-M. (2020) Lumbar Spinal Stenosis: Pathophysiology and Treatment Principle: A Narrative Review, Asian Spine, 14; 5: 682-693.
11. Medline Plus (2016) Medline Plus: Trusted Health Information for You, National Library of Medicine, Degenerative Disc Disease, [Online] https://medlineplus.gov/download/genetics/condition/intervertebral-disc-disease.pdf last visited 11/01/2024.
12. Meyer, F., Börm, W., Thomé, C. (2008) Degenerative Cervical Spinal Stenosis, 105 (20): 366–372.
13. Urban, J. P. G., Roberts, S. (2003) Degeneration of the Intervertebral Disc, Arthritis Res Ther, 5; 120.
14. Xin, J., Wang. Y., Zheng, Z., Wang, S., Na, S., Zhang, S. (2022) Treatment of Intervertebral Disc Degeneration, 14: 1271–1280.
15. Yanagishishita, M. (1993) Function of Proteoglycans in the Extracellular Matrix, 43; 6: 283-293.