The Facial Nerve
- by Joanna Blair
- •
- 05 Jun, 2023
- •
The facial nerve carries sensory information for the anterior two-thirds of the tongue, including taste perception. This gustatory component is the chorda tympani and plays a role in our sense of taste and enjoyment of food.
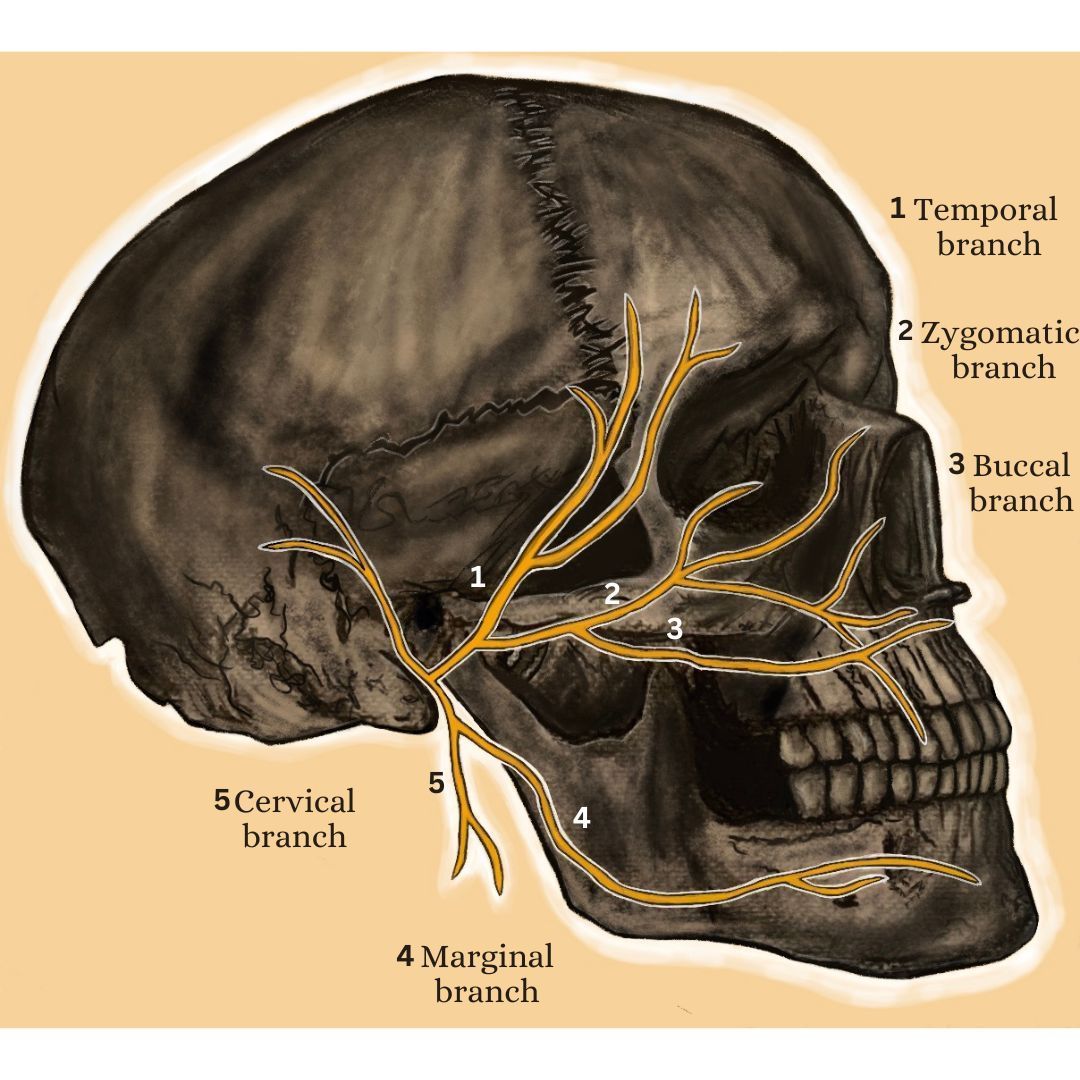
The nerve originates from the brainstem, specifically the pons, and consists of both motor and sensory components. It emerges from the skull through the stylomastoid foramen, a small opening located behind the ear. From there, it travels through a complex course, branching out into various segments that innervate the muscles of the face.
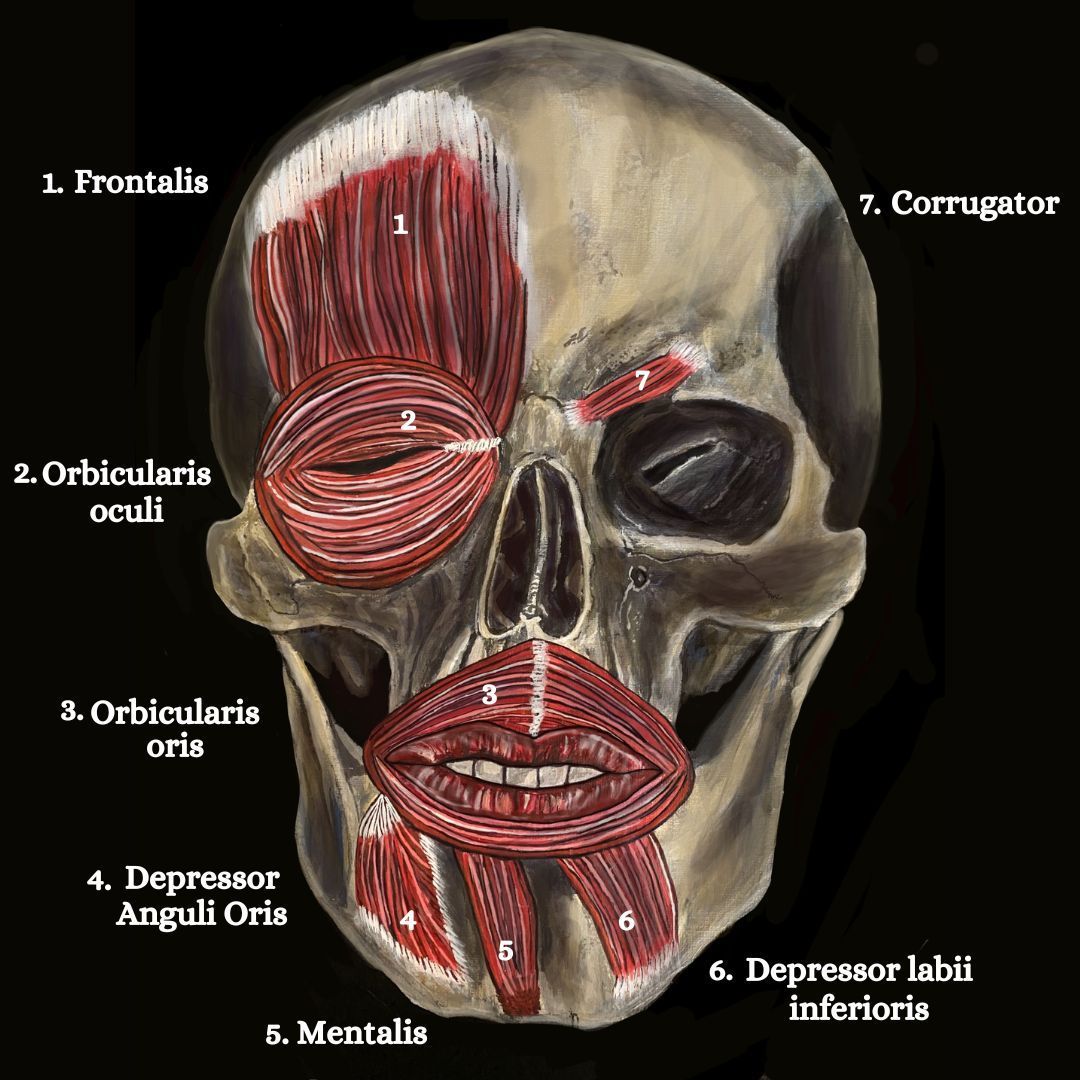
Muscles of the Facial Nerve
Cause
Facial nerve fibres consist of 10,000 neurons, 70% (7,000) of which are motor neurons and 30% (3,000) are sensory. The facial nerve (cranial nerve VII) is responsible for supplying motor innervation to the muscles of facial expression. Here are some of the key muscles supplied by the facial nerve :
1. Frontalis: Located in the forehead and responsible for raising the eyebrows and creating horizontal forehead wrinkles.
2. Orbicularis oculi: Surrounds the eye, closes the eyelids and aids blinking, and squinting.
3. Orbicularis oris: Surrounds the mouth and responsible for lip closure, puckering, and various movements involved in speech and expression.
4. Depressor anguli oris: Lowers the corners of the mouth for frowning expression.
5. Mentalis: elevates the lower lip and the chin.
6. Depressor labii inferioris: pulls the lower lip downward and forward.
7. Corrugator: maintains the position of the brow.
8. Zygomaticus major and minor: Located in the cheek area and involved in smiling and raising the corners of the mouth.
9. Buccinator: This muscle is situated in the cheek and is responsible for compressing the cheeks inward, assisting in activities like blowing air and sucking.
9. Platysma: This muscle extends from the lower jaw to the collarbone and is involved in movements such as lowering the jaw, pouting, and tensing the neck and lower face.
10. Levator labii superioris: This muscle is responsible for elevating the upper lip.
Facial Nerve Palsy (FNP)
Paralysis can occur by pathology anywhere along the facial nerve's peripheral portion and lead to facial nerve palsy (FNP) or Bell's palsy. Bell’s palsy is a neuromuscular idiopathic disorder that affects about 23 individuals per 100,000 per year. The condition causes unilateral facial paralysis and although it can happen at any age, the average age of onset is 40. While the exact cause of Bell's palsy is often unclear, it is believed to result from viral infections such as the herpes simplex virus.
Symptoms include:
- Dry eye
- Facial droop
- Difficulty closing the eyes
- Asymmetrical expressions
- Reduced corneal reflex
- Drooling
- Hyperacusis (sound sensitivity)
- Altered taste
- Otalgia (earache)
- Speech articulation problems
- Difficulty smiling, frowning and expressing emotions
- Tearing of the eye.
- Facial pain.
- Palpebral fissure to expand.
- The nasolabial fold to flatten.
- One corner of the mouth to droop when smiling.
- The eyeball cannot close without moving upward and outward at the same time.
Cause
The cause of paralysis can be due to;
- Vasospasm after exposure to cold or draughts.
- Vascular insufficiency
- Secondary ischemia
- Some form of viral infection.
The risk of Bell’s palsy is increased in patients with hypertension or diabetes and in pregnant women; either late in the pregnancy or in the early postpartum period (4).
Bell’s Palsy and Diabetes Mellitus
Diabetes is associated with as many as 10% of cases and occurs more often in the last trimester of pregnancy (4).
It is possible that diabetic small vessel disease can affect the blood supply of the distal portion of the facial nerve by causing localised facial nerve ischaemia and oedema which is thought to compromise the nerve’s supply by increasing the rigidity of the bony fallopian or facial canal that the facial nerve passes through.
Treatment
The management of facial nerve palsy varies depending on the underlying cause and severity of the condition. In some cases, the nerve may regenerate spontaneously, leading to gradual improvement over time. In more severe cases, various treatment approaches may be employed, including medication, physical therapy, and sometimes surgical intervention.
Surgical Considerations: Due to its intricate course and multiple branches, the facial nerve is vulnerable to injury during certain surgical procedures. Surgeons must exercise caution during surgeries involving the ear, parotid gland, or other adjacent structures to minimize the risk of damage. Preoperative evaluation and meticulous surgical technique are vital in preserving the facial nerve and preventing postoperative complications.
Electrical Stimulation
Current evidence suggests that there is a conflict of opinion for the use of electrical stimulation when treating individuals with Bell’s Palsy. The Bell’s Palsy Association of the United Kingdom discourages the use of electrical stimulation within the early phases of the condition to prevent unintentional damage to muscle fibres (3). Alakram and Puckree (2011) concluded that the application of TENS in the acute stage of Bells palsy is at best, safe and doesn’t interfere with recovery, but is indistinguishable from spontaneous recovery (2).
Facial Massage

1. Encouraging relaxation of taught muscles and encourage stress reduction; Massage therapy can help promote relaxation and reduce stress, which may indirectly benefit individuals with facial nerve injury. Stress can exacerbate muscle tension and increase discomfort, facial massage techniques may help alleviate these symptoms.
2. Increase circulation; massage technique such as effleurage can improve blood circulation in the affected taught areas. This may help deliver oxygen and nutrients to the facial nerves and muscles, promoting healing and reducing inflammation.
3. Muscle Tension Relief; Facial nerve injury can lead to muscle stiffness, spasms, or tension in the face. Massage techniques like kneading, myofascial release, or trigger point therapy may help release tension and reduce muscle tightness, potentially providing relief.
4. Lymphatic Drainage; Facial massage techniques that incorporate gentle, rhythmic movements can assist in lymphatic drainage, promoting the removal of waste products and reducing swelling or edema in the affected area.
However, it's crucial to remember that every facial nerve injury is unique, and the appropriateness and effectiveness of massage therapy may vary. It is essential to consult with a healthcare professional, such as a physical therapist or a specialist in neurology or rehabilitation medicine, who can assess your specific condition and provide appropriate guidance.
Additionally, certain precautions need to be taken when massaging the face, especially in cases of acute or severe facial nerve injury. Applying excessive pressure or manipulating the affected area without proper knowledge or training can potentially worsen symptoms or cause further damage. Therefore, seeking professional advice and guidance is highly recommended to ensure safe and effective treatment.
References
1. Alakram, P., Puckree, T. (2011) Effects of Electrical Stimulation in Early Bell’s Palsy on Facial Disability Index Scores, South African Journal of Physiotherapy, 67; 1: 35-40.
2. Almutairi, S., AlFaris, D., Alshawi, S., Alkhalifah, S., Al Shihri, A., Alshehri, L., Team ENT 435, Facial Nerve [online] https://ksumsc.com/download_center/Archive/4th/435/435%20TeamWork/ENT/F/12-%20Facial%20Nerve%20%28Updated%29.pdf Last visited 31/05/2023.
3. Bharti, N. (2021) Role of Neuromuscular Electrical Stimulation in Bell’s Palsy: A Case Study of Three Patients, International Journal of Science and Healthcare Research, 6; 4: 235-241.
4. Masterson,L., Vallis, M., Quinlivan, R., Prinsley, P. (2015) Assessment and management of facial Nerve Palsy, Education Practice, BMJ, 351; h3725: 32-34. doi: 10.1136/bmj.h3725
5. Pecket, P., Schattner, A. (1982) Concurrent Bell’s Palsy and Diabetes Mellitus: A Diabetic Mononeuropathy; Jounral of Neurology, Neurosurgery and Psychiatry, 45: 652-655.
6. Saxby, E., Kerr, J. (2021) Update on Facial Nerve Palsy: Diagnosis and management of ocular complications, Royal College of Ophthalmologists, Focus [online]