Spinal Stenosis, Sciatica and Lower Back Pain
- by Joanna Blair
- •
- 27 May, 2024
- •

As the Standard noted, sciatica within the elderly is often caused from osteoarthritis within the spine which may cause limited walking distance and cause one's leg to seize after having walked 30 to 40 yards (3).
But, what if sciatica is caused via spinal stenosis? What is the difference between stenosis and osteoarthritis? How can one tell the difference between the two?
Spinal Stenosis
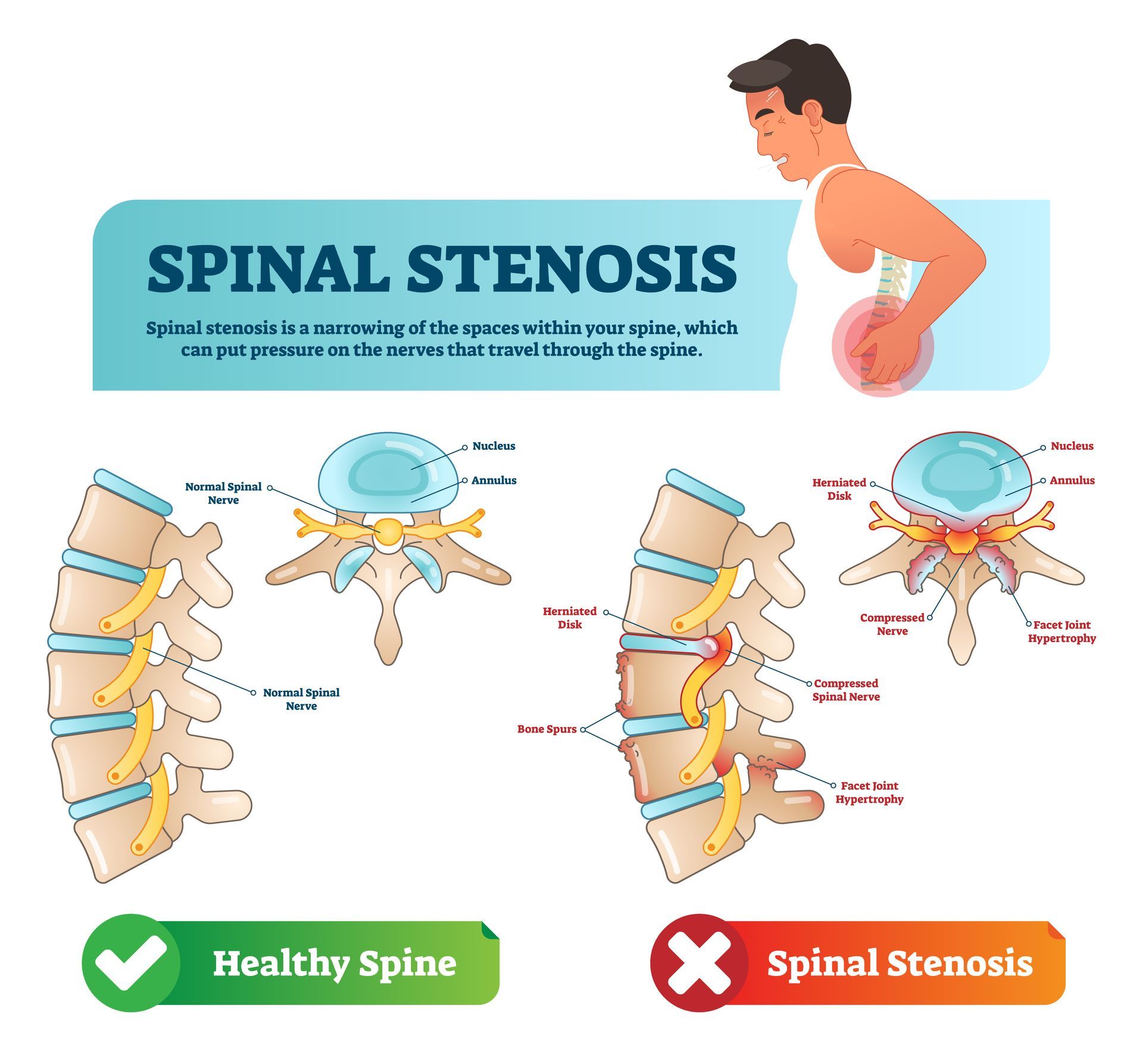
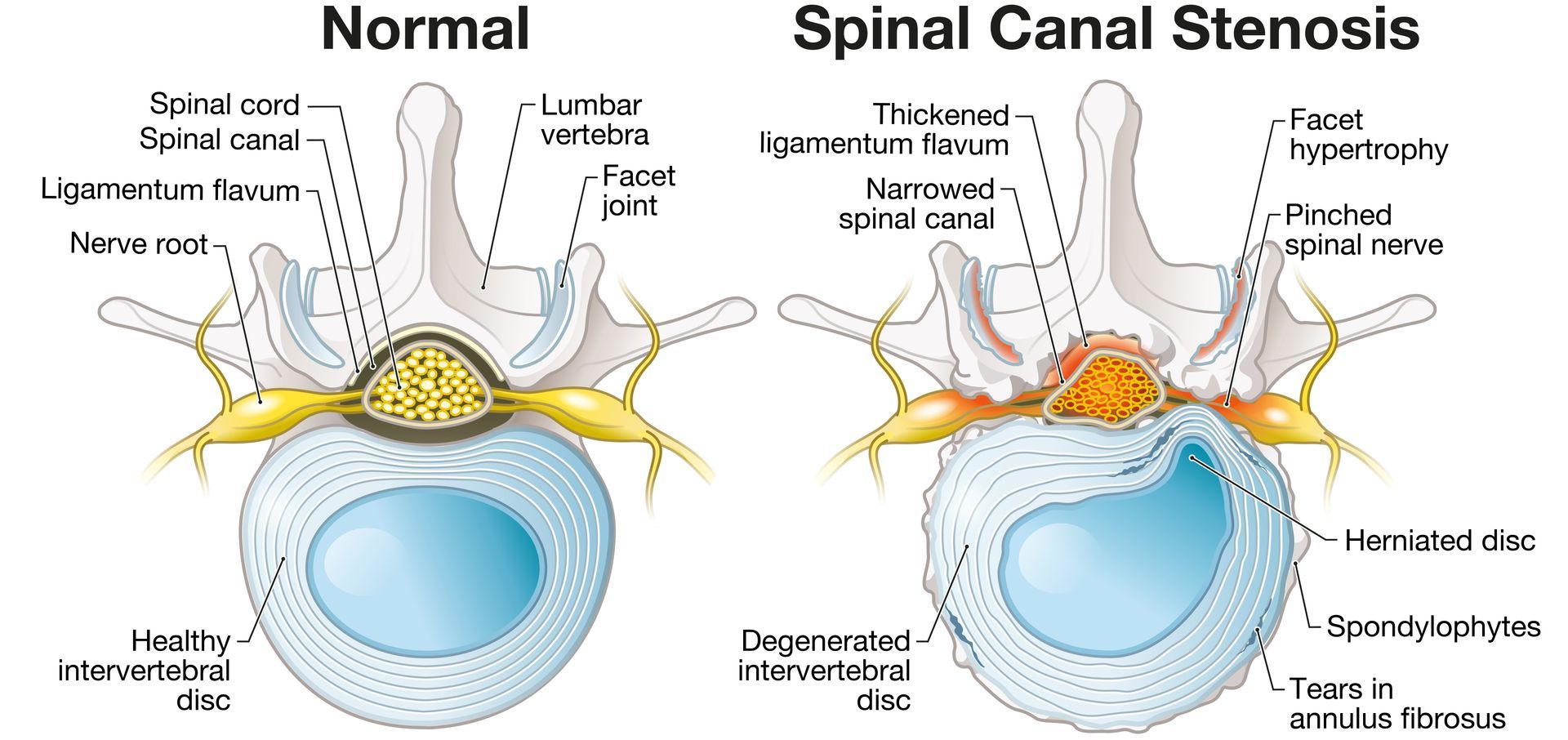
Spinal stenosis is a condition that can cause narrowing of the neural canal and foramina which can result to the compression of the nerve roots and lead to symptoms such as pain, weakness, and numbness (5). The upper neck (cervical) and lower back (lumbar) areas are most frequently affected, although the thoracic spine also can be compressed most frequently by a disc herniation (5). The condition can cause symptoms such as pain, numbness, and weakness (5).
Three different anatomical sites within the vertebral canal can be affected by spinal stenosis (5):
- The central canal, which houses the spinal cord, can be narrowed and lead to compression of neural elements and reduction of blood supply to the spinal cord in the cervical area of the neck and the cauda equina in the lumbar area.
- Secondly, the neural foramen, which are openings through which the nerve roots exit the spinal cord, can be compressed as a result of disk herniation, hypertrophy of the facet joints and ligaments, or unstable slippage of one vertebral body relative to the level below.
- Lastly, the lateral recess, which is seen in the lumbar spine only and is defined as the area long the pedicle that a nerve root enters just before its exit through the neural foramen, can be compressed from a facet joint hypertrophy. Depending on the level of the spine affected, each type of compression can lead to different symptoms that warrant a particular treatment modality.
Most patients will experience some type of pain associated with the spine but luckily, even without surgery, the majority will have an uneventful recovery (6). Only 1 to 3% will have a herniated disc and less than 2% will have compression of a nerve root (6).
Spinal stenosis is common with ageing but predicting which individual will develop symptoms is not possible. In most cases, the degenerative process can be controlled by changes in lifestyle (6).
Lumbar Spinal Stenosis
LSS is a significant cause of disability in older individuals and a common indicator for spinal surgery in patients older than 65 years. Typical, symptoms of lumbar spinal stenosis include (6):
- Pain at the gluteal muscles and/or lower extremities which may or may not be associated with the lower back.
- Neurogenic claudication is a 'hallmark' symptom and characterised by pain in the lower limbs and the presence of neurological symptoms exacerbated by walking.
- In addition, these symptoms are exacerbated by standing and lumbar extension.
Central stenosis arises from anterior ligamentum flavum hypertrophy compounded by posterior disk bulging (4). This condition is more prevalent at the L4 to L5 level than other spinal segments. Meanwhile, lateral recess stenosis can results from facet osteoarthritis (arthropathy) and osteophyte formation that can compress the nerve before it passes the intervertebral foramen.
Foraminal stenosis can result from:
- Disc height loss.
- Foraminal disc protrusion.
- Osteophyte formation.
Physical Therapy For Spinal Stenosis
Simple Lower Back Mobility & Stretch Exercises:
Physical therapy tends to be recommended for patients with mild to moderate LSS (4). Patients with severe LSS typically undergo a trial of conservative treatment before surgery is proposed (4).
Most literature supports the notion that exercise therapy should be considered before surgery. Surgery leads to better longer-term (2 years) outcomes for pain and disability (4).
There is very low-quality evidence to suggest that the two interventions (of surgery and physical therapy) are similar in relation to walking capacity or to pain and disability for the short and long term (4).

Acupuncture For Spinal Stenosis
The therapeutic modality of acupuncture for conservative management of spinal stenosis has historically been met with trepidation, particularly in the Western world (2).
However, clinical trials are beginning to emerge with the majority demonstrating the benefit of acupuncture techniques, particularly electroacupuncture, in providing pain relief in spinal stenosis patients (2).
Acupuncture appears to be a very safe treatment option with several studies demonstrating pain relief at least on par with surgical intervention for patients who do not meet criteria for urgent surgical intervention (2). Clark et al., (2022) concluded that acupuncture appears to be viable and effective as an adjunct conservative treatment option in these patients.
References
1. Ciardi, G., Lamberti, G., Casati, V., Paris, E. (2023) Rehabilitation Outcome Measures in Patients with Spinal Stenosis: A Literary Review, Phsysiologia, MDPI; 3: 421-432.
2. Clark, A., Lucke-Wold, B. P. (2022) Acupuncture and Spinal Stenosis: Considerations for Treatment, HHS Public Access, 1; 1: 23-31.
3. Evening Standard, The Queen is in great pain but insists she will open Parliament, https://www.standard.co.uk/hp/front/the-queen-is-in-great-pain-but-insists-she-will-open-parliament-... [Online].
4.Macedo, L. G., Hum, A., Kuleba, L., Mo, J., Truong, L., Yeung, M., Battie, M. C. (2016) Physical Therapy Interventions for Degenerative Lumbar Spinal Stenosis: A Systematic Review, 93; 12: 1646-1660.
5. Raja, A., Hoang, S., Patel, P., Mesfin, F. B. (2023) Spinal Stenosis, StatPearls Publishing LLC, https://www.ncbi.nlm.nih.gov/books/NBK441989/#:~:text=Most%20patients%20will%20experience%20some,com.... [Online].
6. Wu, L., Munakomi, S., Cruz, R. (2024) Lumbar Spinal Stenosis, https://www.ncbi.nlm.nih.gov/books/NBK531493/ [Online].