Median Nerve Neuropathy & Injury
- by Joanna Blair
- •
- 01 Aug, 2023
- •
Different Sights of Impingement and How Manual Therapy Might Help
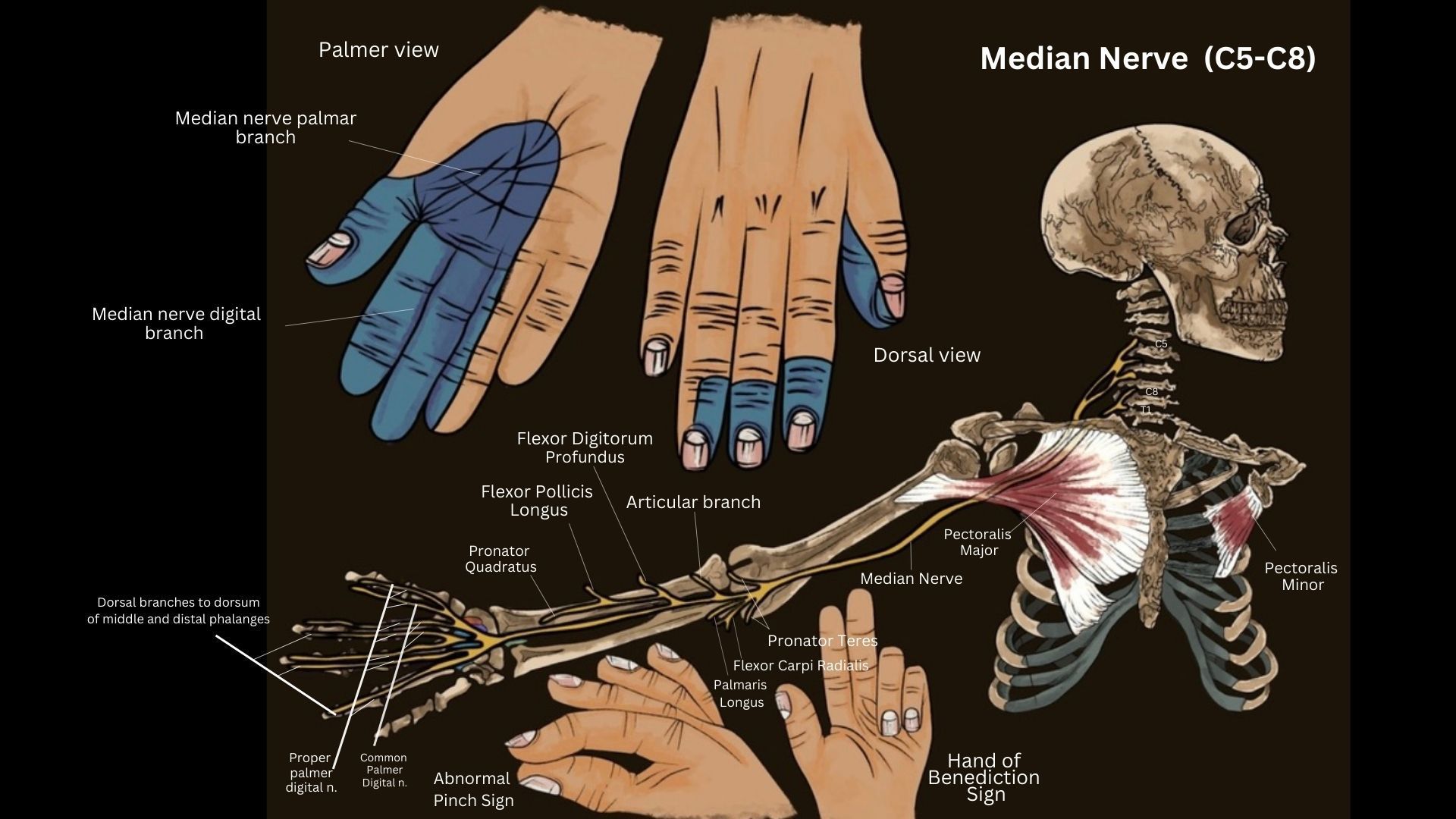
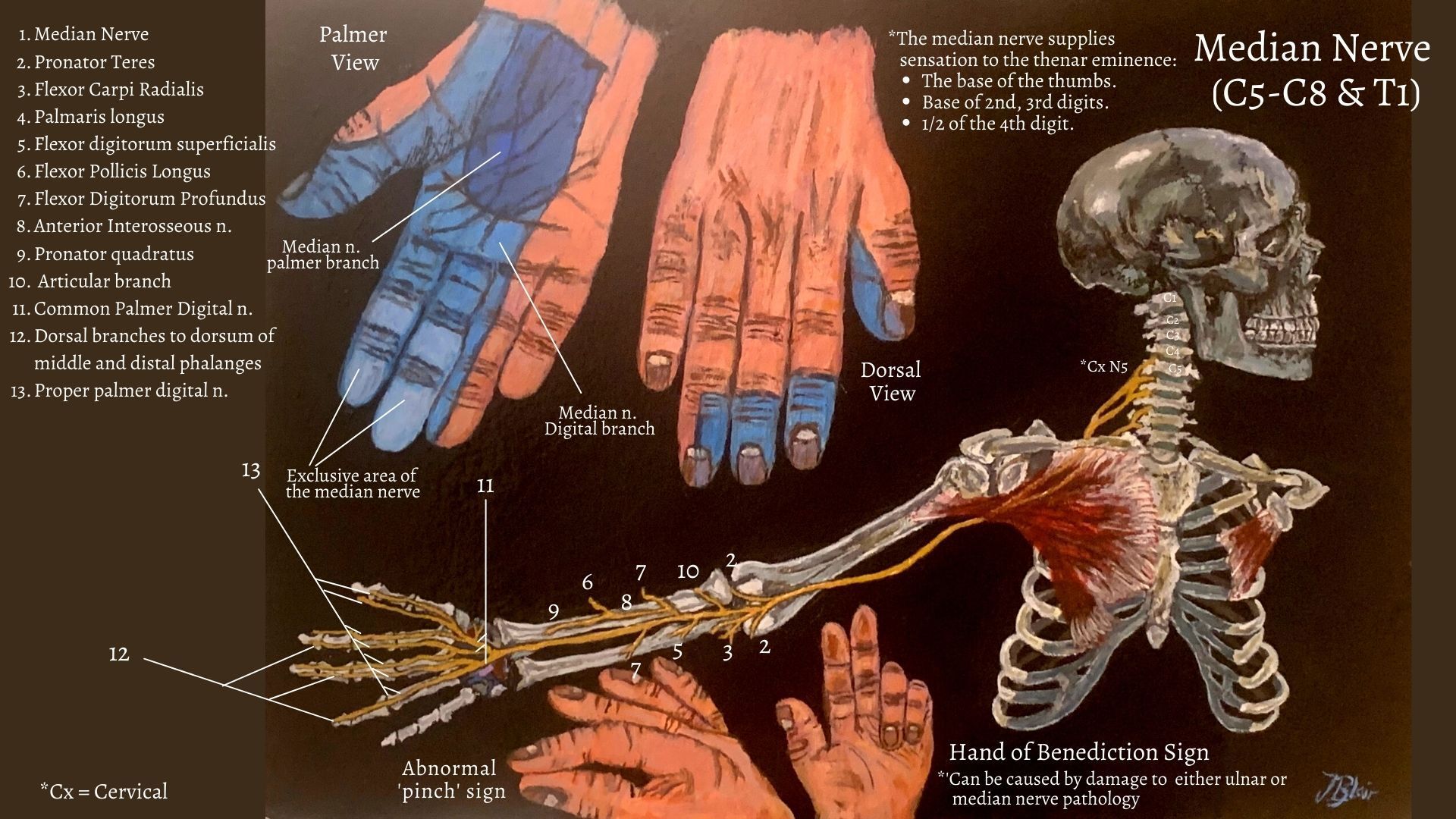
Median nerve injuries are among the most commonly recognized nerve entrapments involving the upper extremity and the primary cause of emergency department access for peripheral nerve injuries. Also referred to as the 'eye of the hand', the median nerve innervates a group of flexor-pronator muscles in the forearm and most musculature in the radial portion of the hand. The nerve controls abduction of the thumb, flexion of the hand at the wrist and flex the fingers.
Anatomy of The Median Nerve
Function of The Median Nerve
The median nerve is a mixed (sensory and motor) nerve. It is classically described as the nerve of pronation, of thumb, index finger, middle finger, and wrist flexion; ofthumb antepulsion and opposition; as well as the nerve of sensation for the palmar aspect of the first three fingers. The median nerve is named so because of its middle position at the end of the brachial plexus and the forearm.
Sensory Innervation of the Median Nerve
Median Nerve injury
Pathology and injury to the median nerve can occur anywhere along the length of the nerve by acute or chronic trauma or compressive lesions which can affect the median nerve at various levels along its long path from the brachial plexus and axilla to the hand.
Peripherally, the median nerve can become compressed under the fascial sheath of the flexor retinaculum, which often causes burning pain, numbness, and tingling (neuropathic pain) commonly known as carpal tunnel syndrome (CTS). CTS is the most commonly recognised entrapment neuropathy and can be further read in another post here. It is worth to noting that CTS is idiopathic and also associated with hypothyroidism, pregnancy, and diabetes. This article will concentrate on investigating other entrapment sites of the median nerve and how it may affect the innervated arm.
Median Nerve Entrapment at the Elbow
1. The distal humerus by the ligament of Struthers.
2. Proximal elbow by a thickened biceps aponeurosis.
3. Deep heads of pronator teres muscle.
4. Proximal forearm via flexor digitorum superficialis muscle.
This blog will specifically study the following syndromes and link the above listed with association to the median nerve:
1. Ligament of Struthers syndrome
2. Pronator Teres Syndrome
3. Lacertus Tunnel Syndrome
4. Anterior Interosseous Nerve Syndrome
The Ligament of Struthers Syndrome
Lacertus Tunnel Syndrome
The most common complaints in patients with lacertus syndrome are:
- A loss of tip pinch strength
- Reduced fine motor skills and sense of clumsiness (dropping objects).
- Burning sensations and numbness in the palmar cutaneous branch of the median nerve distribution.
- Weakness when manually testing the strength of the muscles innervated by the median nerve distal to the lacertus fibrosus, especially the FPL, FDP II, and FCR.
- External pressure of the median nerve at the level of the lacertus fibrosus will elicit distinct pain and, at times, a positive Tinel’s sign.
Pronator Teres Syndrome
The anterior interosseous nerve is a purely motor nerve and supplies the pronator quadratus muscle, flexor muscles of the forearm and muscles for the index and middle fingers. This syndrome mimics CTS, but it does not respond to splinting, NSAIDs, steroid injection, or carpal tunnel surgery.
Symptoms
Patients with pronator syndrome present with pain and paresthesia (pins and needles) within the elbow, forearm and hand affecting the thumb to middle fingers and lateral half of the ring finger. The most common distribution of sensation is loss within the lateral palm and sensory loss over the thenar eminence (base of the thumb).
The hand symptoms are similar to carpal tunnel syndrome and both syndromes may be aggravated by overuse. Pronator syndrome can be associated with numbness of the palm because of compression of the palmar cutaneous nerve, whereas symptoms that wake the patient at night are more common with carpal tunnel syndrome.
Tinel sign should be positive over the wrist in patients with carpal tunnel syndrome, whereas it is positive over the elbow and proximal forearm in patients with pronator syndrome. In addition, symptom reproduction during resisted forearm pronation suggests median nerve compression by the pronator teres compared to symptom reproduction during resisted elbow flexion and supination, suggesting biceps aponeurosis as the cause of compression.
Clinic Presentation
The clinical presentation is typically aching pain in the hand/wrist with activities involving sustained pronation, such as typing, writing, using a mouse or cell phone, or driving a car. The pain is in the distribution of the terminal, sensory branch of the AIN (i.e., the volar wrist). As the syndrome progresses, patients may complain of numbness in the entire hand, particularly at night, especially with any pressure on the proximal forearm or about the medial elbow. In theory, a way to differentiate CTS from pronator teres syndrome is the presence of sensory symptoms in the thenar eminence at the base of the thumb. The pronator teres is ironically spared in pronator teres syndrome and it is important to note that there are no symptoms at the site of nerve compression, but rather where the cutaneous nerve ends.
The condition can often be observed in individuals who perform certain actitivities in different trades such as regular and daily use of screw drivers. Asking individuals to extend the elbow with repeated pronation of the forearm can often reproduce symptoms of pronator syndrome.
The syndrome is also seen in professional cyclists. Treatment of pronator teres syndrome includes limiting activity that produces symptoms. NSAIDs, local corticosteroid injections into the tender points of pronator teres, and median nerve decompression surgery have also demonstrated effectiveness.
Anterior Interosseous Nerve Syndrome (AINS) & 'OK' Sign
Injury
Damage or compression of AIN causes anterior interosseus nerve syndrome (also called the Kiloh-Nevin syndrome) which causes a palsy of the three muscles that the nerve supplies. The three muscles are flexor pollicis longus (which flexes the thumb at the distal phalanx), pronator quadratus (causing pronation at the radioulnar joint) and the radial half of flexor digitorum profundus (creates flexion of the index and middle fingers).Neuropathy of the AINS nerve presents with muscular weakness with no sensory deficits. Traumatic causes of the syndrome include penetrating injuries, fracture at the level of the forearm and cast fixation. Compression of the nerve can be due to nerve entrapment in pronator teres, occlusion of the radial or ulnar artery, and enlarged bicipital tendon bursa.
Presentation - The 'OK' Sign
Patients with AINS are unable to pinch objects or make a clear "OK" sign with their index finger and thumb. The “O” sign is otherwise acheived via the index finger and thumb (via flexor pollicis longus). Upon physical examination, the patient is unable to approximate the thumb and index finger. An injury to the anterior interosseous nerve most commonly occurs with complex trauma.
Patients with anterior interosseous nerve (AIN) syndrome, after the two authors who described the syndrome in 1952 observed motor weakness typically manifested by weakened ability to pinch the thumb and index finger together, tested by asking the patient to make an “OK” sign withthe hand, reflecting the palsy of the flexor pollicis longus muscle and flexor digitorum profundus muscle to the index finger.
Sources read do state that this sign should not purely be relied upon to make this diagnosis and to test for strength of the flexor pollicis longus.
The pinch grip test is positive and the patient cannot demonstrate an “OK” sign which is possible when the Anterior interosseous nerve is intact. Sensory loss is not present in the case of anterior interosseus nerve syndrome (AINS) which differentiates it from other nerve palsies such as carpal tunnel syndrome and pronator syndrome.
Treatment:
Surgical treatment is needed for patients who do not show any improvement with anterior interosseus nerve syndrome during the first three months. Decompression of the nerve is necessary at the compression site. There is no proper treatment and the diagnosis is made with the help of MRI and the presenting complaints by the patient.
Treatment
Physical Therapy & Exercise
Conservative therapies include physical therapy, yoga, and therapeutic ultrasound. Again, first-line for conservative management in the case of mild to moderate carpal tunnel are corticosteroid injections and night splints. Massage application, acupuncture or electrotherapy might be used to help reduce tensions within the related muscles mentioned above particularly within the forearm, upper back and neck.
Surgical Intervention
Proximal median nerve release is considered if symptoms persists when conservative treatment prevention has been unsuccessful. The consideration of relevant structures to be incisionally released via surgical measures include; the fascia of Struthers, the bicipital aponeurosis, the deep fascia of the ulnar origin of the pronator teres and the fascial arch of the superficial flexors (6).
Use of Wrist Splinting
Management of median nerve injury depends on the etiology. Splinting is considered a first-line treatment option for mild to moderate carpal tunnel. Research shows it to be superior to placebo, but no single splint stands out as superior. However, a separate study has shown a neutral wrist splint to be twice as effective in symptomatic relief compared to that of an extension splint. If initially starting with night splints, and the patient does not have relief after one month, the recommendation is to continue for another one to two months but add another conservative treatment modalities to the care plan. Splints can be worn at night or continuously, but have continuous use has not been shown to be superior to night time wearing the splint.
Corticosteroid Injection
A local corticosteroid injection has been shown to delay the need for surgery at one-year following an injection. The risks of a local corticosteroid injection include possible injection into the median nerve as well as tendon rupture. The recommendation is to do a carpal tunnel injection under ultrasound guidance to limit risks and improve the accuracy of the injection. A repeat corticosteroid injection may be offered six months following the initial injection. If symptoms recur after the second injection, then surgery is recommended to be considered.
References
(2021) The Myth of Median Nerve in Forearm and Its Role in Double Crush Syndrome: A Cadaveric Study, Frontiers in Surgery; 8: 1-8.
2. Caetano, E. B., Neto, J. J. S., Vieira, L. A., Caetano, M. F., de Bona, J. E., Simonatto, T. M. (2017) Struthers' Ligament And Supracondylar Humeral Process: An Anatomical Study And Clinical Implications; Acta Ortop Bras; 25 (4): 137-42.
3. Dydyk, A. M., Negrete, G., Cascella, M. (2021) Median Nerve Injury, https://www.ncbi.nlm.nih.gov/books/NBK553109/ [online]
4. Lalonde, D. (2015) Lacertus syndrome: a commonly missed and misdiagnosed median nerve entrapment syndrome,
5. Miller, T. T., Reinus, W. R. (2010) Nerve Entrapment Syndromes of the Elbow, Forearm, and Wrist, AJR; 195: 585-594.
6. Singh, V., Ericson, W. B. (2016) Median Nerve Entrapments (Chapter 37); Peripheral Nerve Entrapments: Clinical Diagnosis and Management, Springer International Publishing, Switzerland: 369-382.